Subscribe now to get notified about IU Jharkhand journal updates!
Belief and Attitude of General Physicians of West Bengal towards Early Initiation of Insulin Therapy in Type 2 Diabetes Patients- a Descriptive approach; and build the Best Fit Belief-Behaviour Model
Abstract :
Diabetes is a progressive disorder, and patients currently on three or more oral drugs, going
ahead will inevitably require insulin therapy to attain and maintain adequate glycaemic control.
It is a known fact that pancreatic beta cells are already quite exhausted at this case, and in order
to make them optimally respond to oral drugs at a later stage, they must be given some rest,
and hence exogenous initiation of insulin is a must to do task in hand without any further
delay. But in reality, insulin initiation is a big challenge and is delayed in many patients who
would otherwise benefit from such treatment. Patients' and Physicians' beliefs' perceptions,
and attitude regarding insulin therapy are known to create barriers contributing to their
reluctance and subsequent delay in its initiation. This article studies the different factors
(explanatory variables) pertaining to their belief and attitude, and their degree of impact on
initiation of insulin; It also aims to provide practical solutions for addressing and overcoming
these hurdles so that insulin can be initiated confidently in order to improve diabetes treatment.
Keywords :
Belief and Attitude, Early initiation of insulin therapy, Barriers to Insulin initiation, Belief-Behaviour model.1. Introduction
Insulin is the most effective drug available to achieve glycemic target in OAD (Oral Anti-Diabetic Drugs) failure Type 2 DM patients. All global guidelines also recommend starting insulin early in order to get a sustained and optimal glycemic control. The term OAD failure refers to the clinical state when all of the following criteria are met:
(i) HbA1C above goal (≥7%) despite concurrent and use of 3 OADs.
(ii) OAD classes should be different; one should be Metformin and the second a Sulphonylurea.
(iii) Adequate lifestyle control measures have been followed.
(iv) Comorbid conditions causing hyperglycemia have been ruled out.
Ref: Jindal, S., & Kalra, S. (2020). Developing a definition for Oral Antidiabetic Drug (OAD) Failure. JPMA, 2019.
Initiation of insulin impacts the metabolic memory in a positive way and generates a legacy that delays the long term complications. As per UKPDS Study, by the time diabetes is diagnosed, almost 50% of the Pancreatic Beta cells are destroyed. So, the more we delay, the more is the chance of micro and macro-vascular complications; hence the earlier, the better it is. Yet, there is reluctance and aversion among the physicians (specifically primary care physicians) in West Bengal to initiate insulin therapy early in these patients. Majority of the Primary care physicians lack conviction in early initiation of insulin therapy after 2 oral drugs, and instead wait till 4 oral drugs, thus increasing the risk of long term complications in Type 2 Diabetes Patients. Hence it becomes pertinent and prudent to understand the causal-effect relationship between early initiation and the various contributing factors behind this.
OBJECTIVES OF THE STUDY:
- To understand the General Physicians’ (Customers) beliefs and attitudes about Early Initiation of insulin in Type 2 DM patients.
- To find the degree of correlation between Early initiation of insulin therapy and the various factors contributing behind this decision making, i.e., how strongly each factor affects the customer buying decision.
- To build a linear regression model in order to fit a linear relationship between Early initiation (Response/ Dependent variable) and the set of various factors (Explanatory/ Independent variables), which might affect the decision making and interpret each of those coefficients.
SCOPE OF STUDY
India is called the Diabetes Capital of the World. The diabetic population in the country is close to hitting the alarming mark of 75 million by 2025 and 80 million by 2030. As per WHO report published on 10-Oct-2019 (INDIAB Study), there are estimated 72.96 million cases of diabetes in adult population of India. The prevalence in urban areas ranges between 10.9% and 14.2%, and prevalence in rural India was 3.0-7.8% among population aged 20 years and above with a much higher prevalence among individuals aged over 50 years.
Estimated by the International Diabetes Federation in 2017, the prevalence of diabetes among the adults (20–79 years of age) in India is 72.9 million. https://care.diabetesjournals.org/content/42/3/476#ref-1
A phenomenal increase in diabetes from 40.9 million in 2007 to 72.9 million in 2017 (~2 fold) occurred. The prevalence is likely to increase further by 1.84-fold, i.e., to 134.3 million by 2045. Once again, India is likely to have the largest number of people with diabetes in the world. The prevalence of impaired glucose tolerance (IGT) is 2.9% (24 million). https://care.diabetesjournals.org/content/42/3/476#ref-1
Asian countries, specifically, India and China, are undergoing rapid socioeconomic progress and are susceptible to many adverse consequences such as unhealthy lifestyle leading to high prevalence of diabetes and other non-communicable diseases. https://care.diabetesjournals.org/content/42/3/476#ref-2
Epidemiological studies in India since 1980 have highlighted the changing trends in prevalence of diabetes, pre-diabetes, and associated risk factors https://care.diabetesjournals.org/content/42/3/476#ref-6
LIMITATIONS AND SCOPE FOR FUTURE WORK:
This is a general study which is done on the population of Primary care General Physicians, with
Factors which are not being considered are Academic inclination of HCP and Geographic area of
practise (rural/urban). The results of this study may vary fairly to some extent when the above two
factors are taken into consideration. Thus it keeps the scope open for future work on the same.
LITERATURE REVIEW:
As per Hayes et al, PCPs share some beliefs about initiating insulin; there is a lack of consensus about
other aspects of insulin therapy. Most shared beliefs fall into one of four categories: benefits of insulin
therapy vs. risks, positive experiences of patients on insulin, fears or concerns of patients still on oral
therapy, and the management of and training for insulin use.
The majority of PCPs agreed that the benefits of using insulin to prevent or delay complications
outweighed the risks of hypoglycemia and weight gain for most patients. However, there were fewer
consensuses when the patient was severely obese or elderly. For example, while the clear majority of
PCPs agreed that the benefits of insulin outweighed the risks of hypoglycemia for most patients, 44%
agreed that the risk of hypoglycemia made them reluctant to prescribe insulin to most patients who were 85 years old
Ref: Hayes, R. P., Fitzgerald, J. T., & Jacober, S. J. (2008). Primary care physician beliefs about insulin
initiation in patients with type 2 diabetes. International Journal of Clinical Practice, 62(6), 860-868.
As per United Kingdom Prospective Diabetes Study (UKPDS), early initiation of insulin impacts the metabolic memory in a positive way and generates a legacy that delays the long term complications. By the time diabetes is diagnosed, almost 50% of the Pancreatic Beta cells are destroyed. So, the more we delay, the more is the increased chance of micro and macro-vascular complications.
Ref: Chalmers, J., & Cooper, M. E. (2008). UKPDS and the legacy effect.
The relative contribution of postprandial glucose excursions is predominant in fairly controlled patients, whereas the contribution of fasting hyperglycemia increases gradually with diabetes worsening. The higher the HbA1C, the more is the contribution of Fasting Blood Glucose. Hence it becomes very necessary to fix the Fasting first.
Ref: Monnier, L., Lapinski, H., & Colette, C. (2003). Contributions of fasting and postprandial plasma glucose increments to the overall hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA1c. Diabetes care, 26(3), 881-885.
As per the LANDMARC (Longitudinal Nationwide Study on Management And Real World Outcomes of Diabetes in India) Trial, which is Largest Nationwide Prospective Longitudinal Observational Study done on 6236 participants and at 382 sites across India.
(i) Less than 20% Type 2 DM patients achieve optimum control in India.
(ii) Less than 20% patients receive insulin therapy even after diagnosis of more than 8 years.
(iii) Adding more than 3 OADs does not offer additional glycemic improvement.
Ref: Das, A. K., Mithal, A., Kumar, K. M. P., Unnikrishnan, A. G., Kalra, S., Thacker, H., & Joshi, S. (2020). Rationale, study design and methodology of the LANDMARC trial: a 3‐year, pan‐India, prospective, longitudinal study to assess management and real‐world outcomes of diabetes mellitus. Diabetic Medicine, 37(5), 885-892.
As per the results of Ellis et al study, twelve key themes were identified and formed three domains, patient perceptions, healthcare professional perceptions, and health professional-patient relationships. The patient-centred themes were: insulin-related beliefs, social influences, psychological factors, hypoglycaemia, and therapy barriers. The clinician-related themes were: insulin skills of general practitioners, healthcare integration, healthcare professional-perceived barriers, hypoglycaemia, and explanations for adherence. Healthcare professional-patient relationship themes were drawn from the perspectives of patients and from clinicians. This review reveals multiple barriers to optimal insulin use in primary care at both the patient and healthcare professional levels. These barriers indicate the need for multimodal interventions to: improve the knowledge and competencies of primary care professionals in insulin use; provide more effective patient education and self-management support; and introduce integrated insulin support systems.
Ref: Ellis, K., Mulnier, H., & Forbes, A. (2018). Perceptions of insulin use in type 2 diabetes in primary care: a thematic synthesis. BMC family practice, 19(1), 1-21.
As per the DiabCare India 2011 study, more than 15% physicians felt that the greatest barrier to insulin therapy from patient's perspective were pain and fear of using injectable modality; 5.2% felt that the greatest barrier to insulin therapy from physician's perspective was the treatment cost; 4.8% felt that the major barriers to achieve optimum diabetic care in practice was loss to follow-up followed by lack of counselling (3.9%) and treatment compliance (3.6%).These results indicate a need for more structured intervention at an early stage of the disease and need for increased awareness on benefits of good glycaemic control.
Mohan, V., Shah, S. N., Joshi, S. R., Seshiah, V., Sahay, B. K., Banerjee, S., ... &DiabCare India 2011 Study Group. (2014). Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: results from the DiabCare India 2011 Study. Indian journal of endocrinology and metabolism, 18(3), 370.
According to United Kingdom Prospective Diabetes Study by Holman, the durability of the glycemic control obtained is dependent on the degree to which beta-cell function can be maintained; despite an initial upward trend, Beta-cell mass reduces progressively at 4% per year with conventional OADs monotherapy.
Holman, R. R. (2006). Long-term efficacy of sulfonylureas: a United Kingdom Prospective Diabetes Study perspective. Metabolism, 55, S2-S5.
❖ RESEARCH DESIGN TARGET POPULATION:
The set of all Primary Care General Physicians practising in Kolkata city and the surrounding districts of West Bengal, with a practice of >= 10 years. SAMPLING DESIGN:
Sample size: 200
From the target population, the Sampling frame for this study is the list of (only) MBBS degree holder Primary Care physicians (with or without a Diploma in Diabetes), practising for ≥10 years, and having age between 35and 45 years of age (each being referred to as a sampling unit).
Initially, Purposive and Deliberate Sampling is applied to deliberately choose the Sampling units as MBBS degree holder Primary Care General Physicians(with or without Diploma in diabetes), practicing for ≥ 10 years, and 35 ≤Age ≤ 45 years from the entire population of General physicians, thus forming the Sampling Frame from the target population.
And then Simple Random Sampling is applied to randomly pick 200 respondents from this Sampling frame. Hence, every single sampling unit in the sampling frame stands an equal chance to get picked (irrespective of gender and region, social and demographic status), so that whatever be the end results, we can attribute them to have happened purely by chance, and there is no bias involved.
OBSERVATIONAL DESIGN:
The entire research study is conducted under a Simulated environment, where the respondents are completely aware of the study.
PRIMARY DATA COLLECTION:
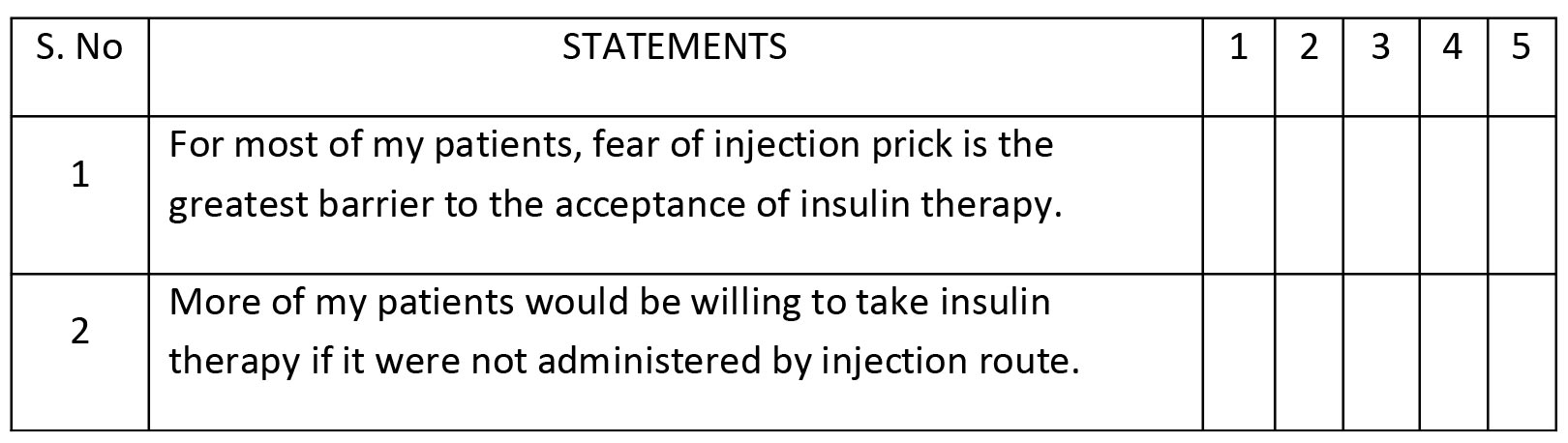
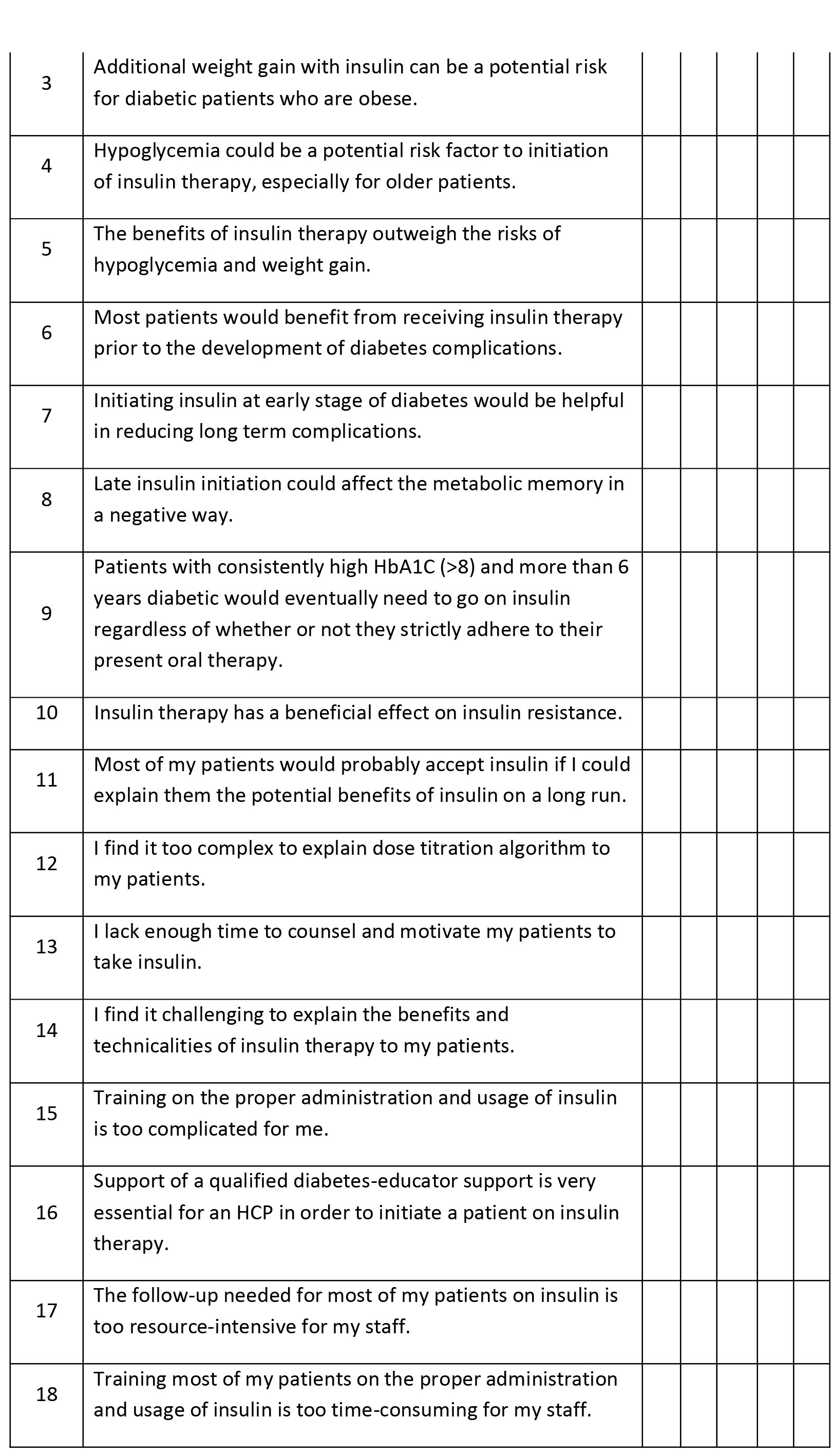
❖ STRUCTURED QUESTIONNAIRE A Structured Questionnaire containing 28items/ statements is given to all of the 200 participants, wherein each statement (indicating towards a particular Construct), requires to express their opinion or belief on a 5-Point Likert Scale ranging from 1 as ‘Strongly disagree’ to 5 as ‘Strongly Agree’.
QUESTIONNAIRE SURVEY
(i) Total volume of patients seen in a month who are already on >=3 OADs and yet uncontrolled:_______________
(ii) No. of patients initiated on Insulin in a month : __________
Please tick the appropriate column to rate the following statements on a scale of 1 to 5, 1 being the “STRONGLYDISAGREE” and 7 being the “STRONGLY AGREE” as depicted below:
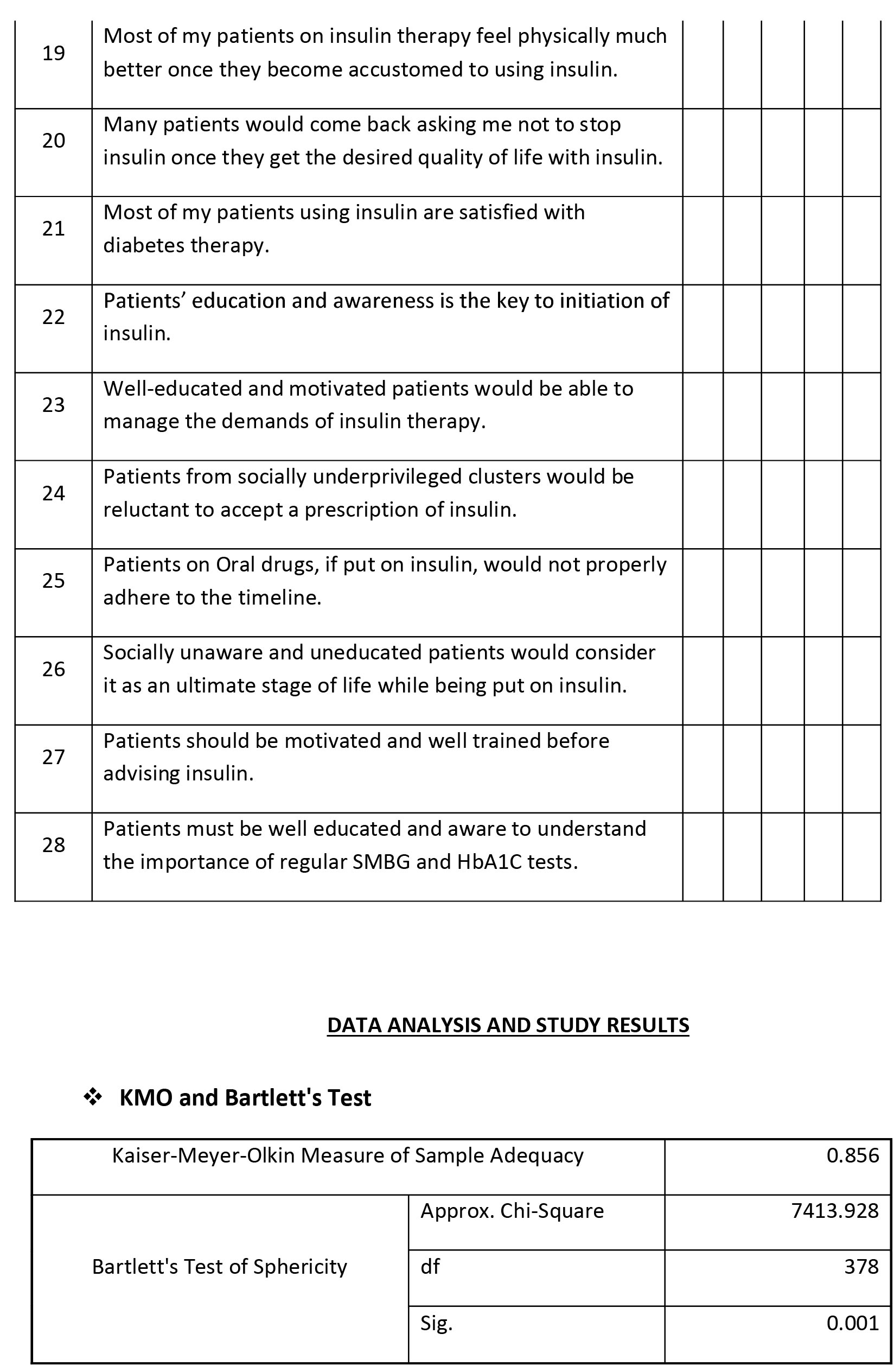
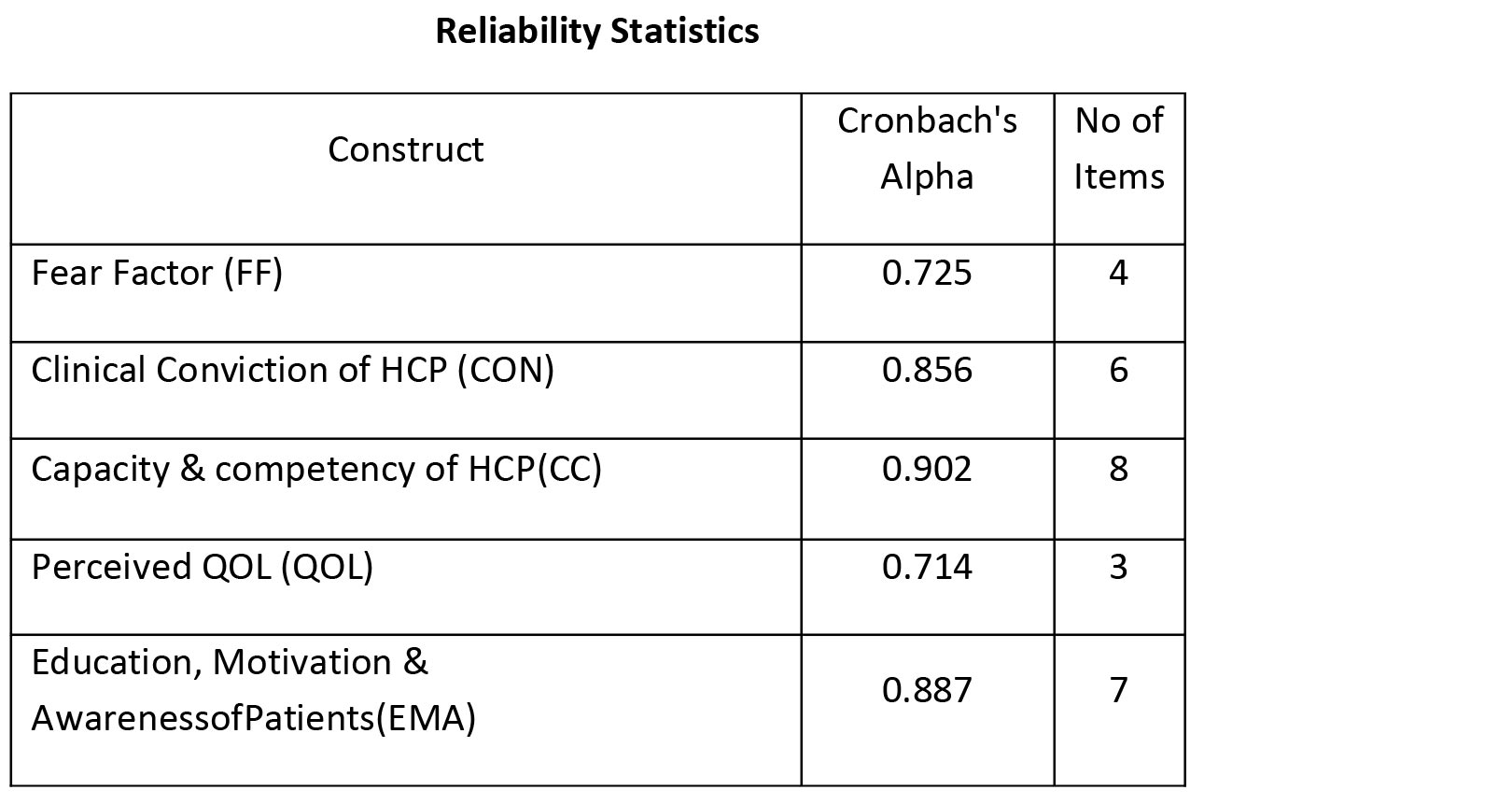
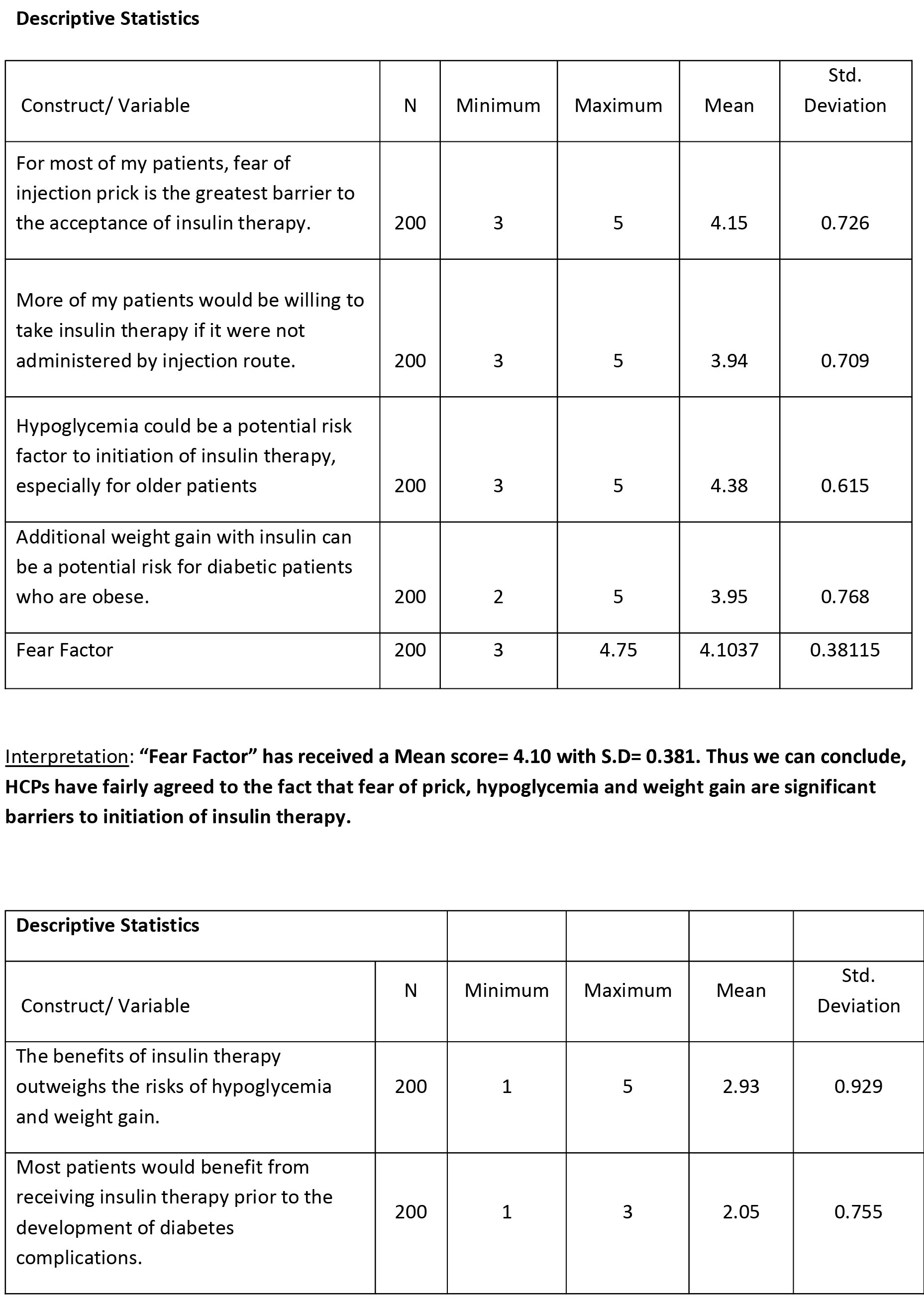
Interpretation of Test Result:
❖The obtained KMO value of 0.856 indicates that the sample is adequate to proceed further and do the Factor Analysis.
❖The Bartlett’s test of Sphericity is used to test the following hypotheses: Null Hypothesis, H(0): Variables are Not Correlated (i.e., Orthogonal), i.e., there is no significance difference between the Correlation matrix and the Identity matrix, as against the Alternative Hypothesis, H(a): Variables are Correlated (i.e., Not Orthogonal), i.e., the Correlation Matrix significantly differs from Identity matrix. The obtained p-value (=0.001) < chosen significance level of 0.05, which allows us to reject our Null Hypothesis, and infer that the variables are correlated, i.e., the Correlation Matrix differs significantly from the Identity Matrix; and hence we get a green signal to proceed further with our dataset to subject it to Principal Component Analysis or Factor Analysis.
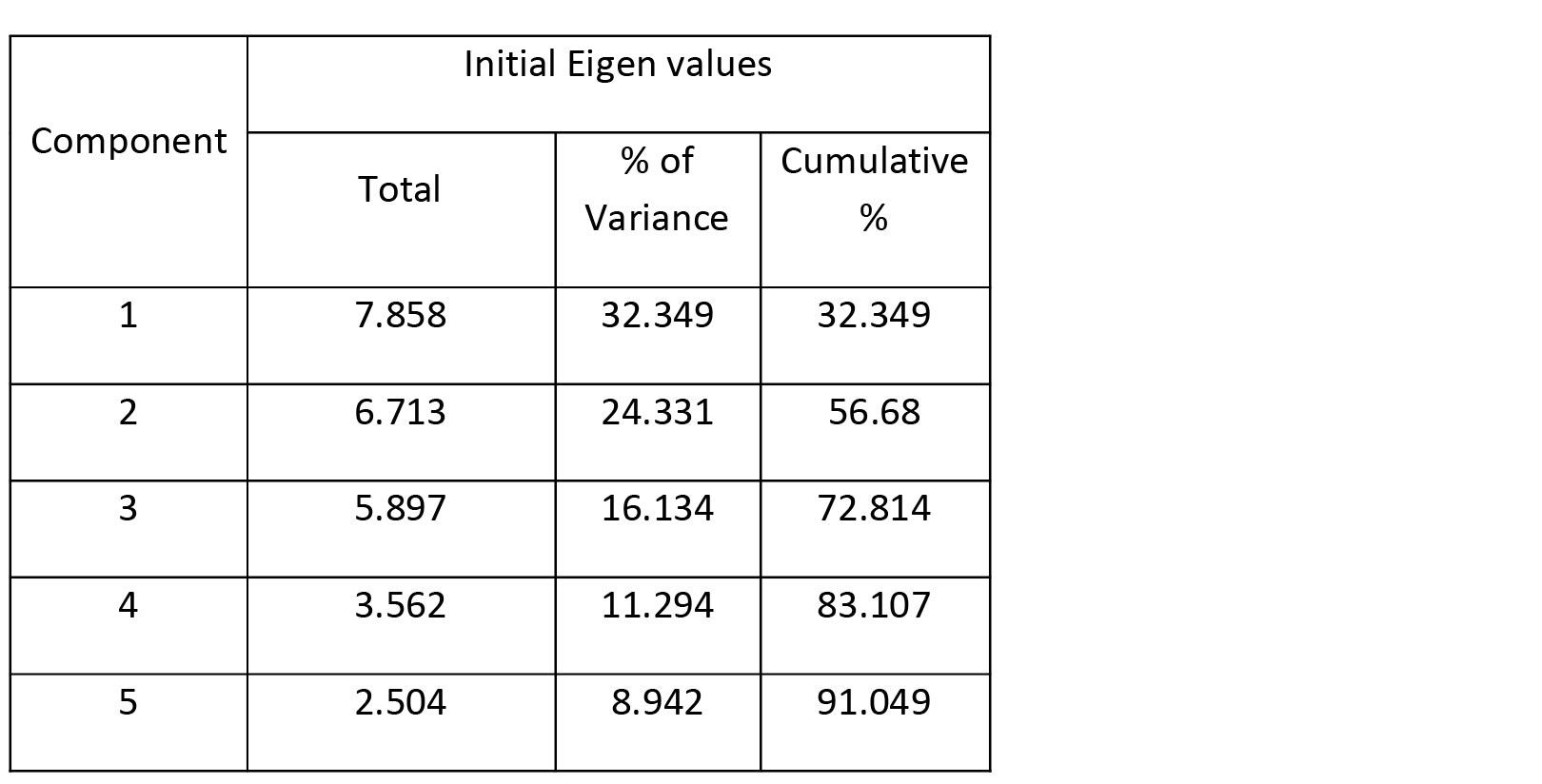
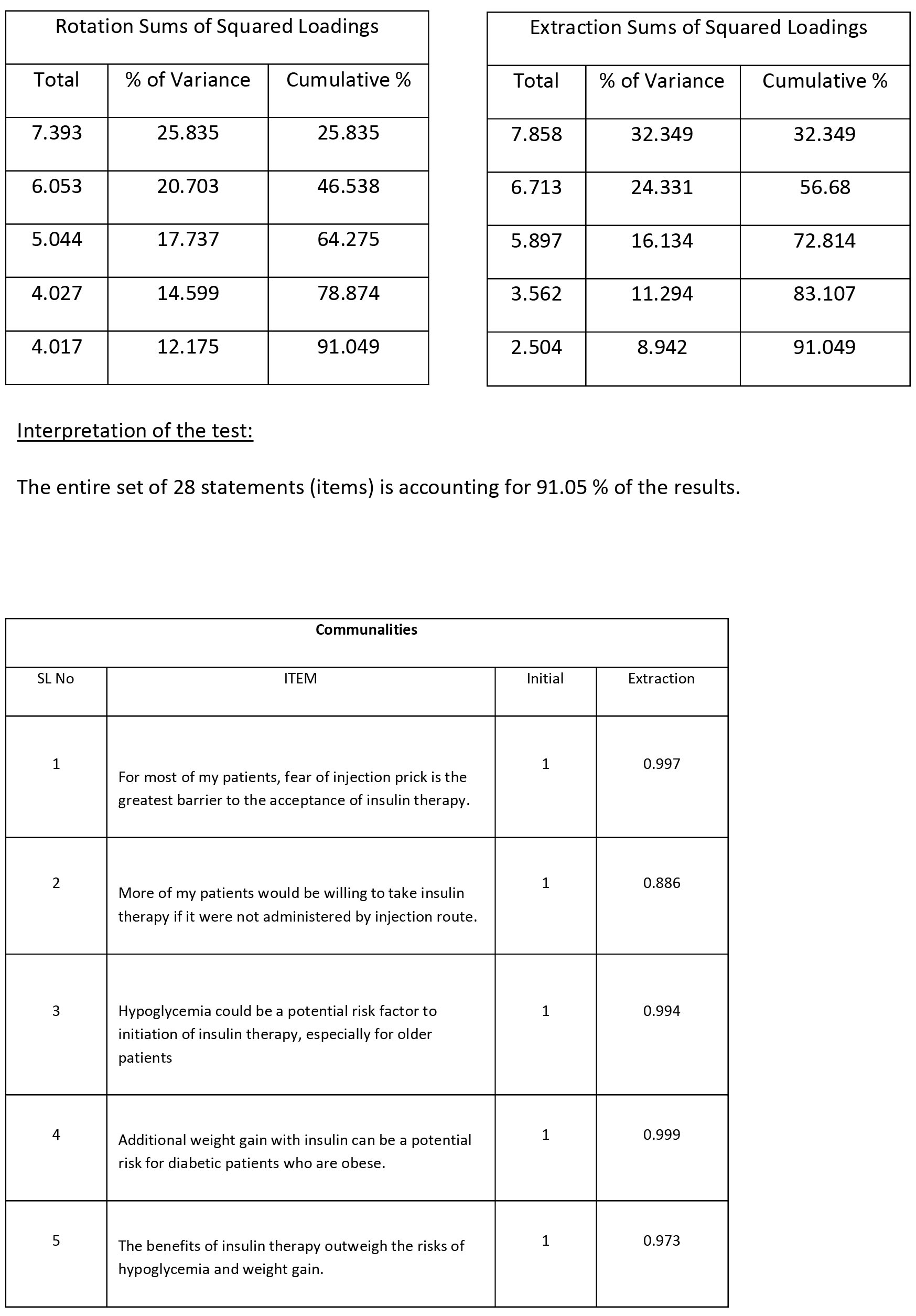
Extraction Method: Principal Component Analysis.
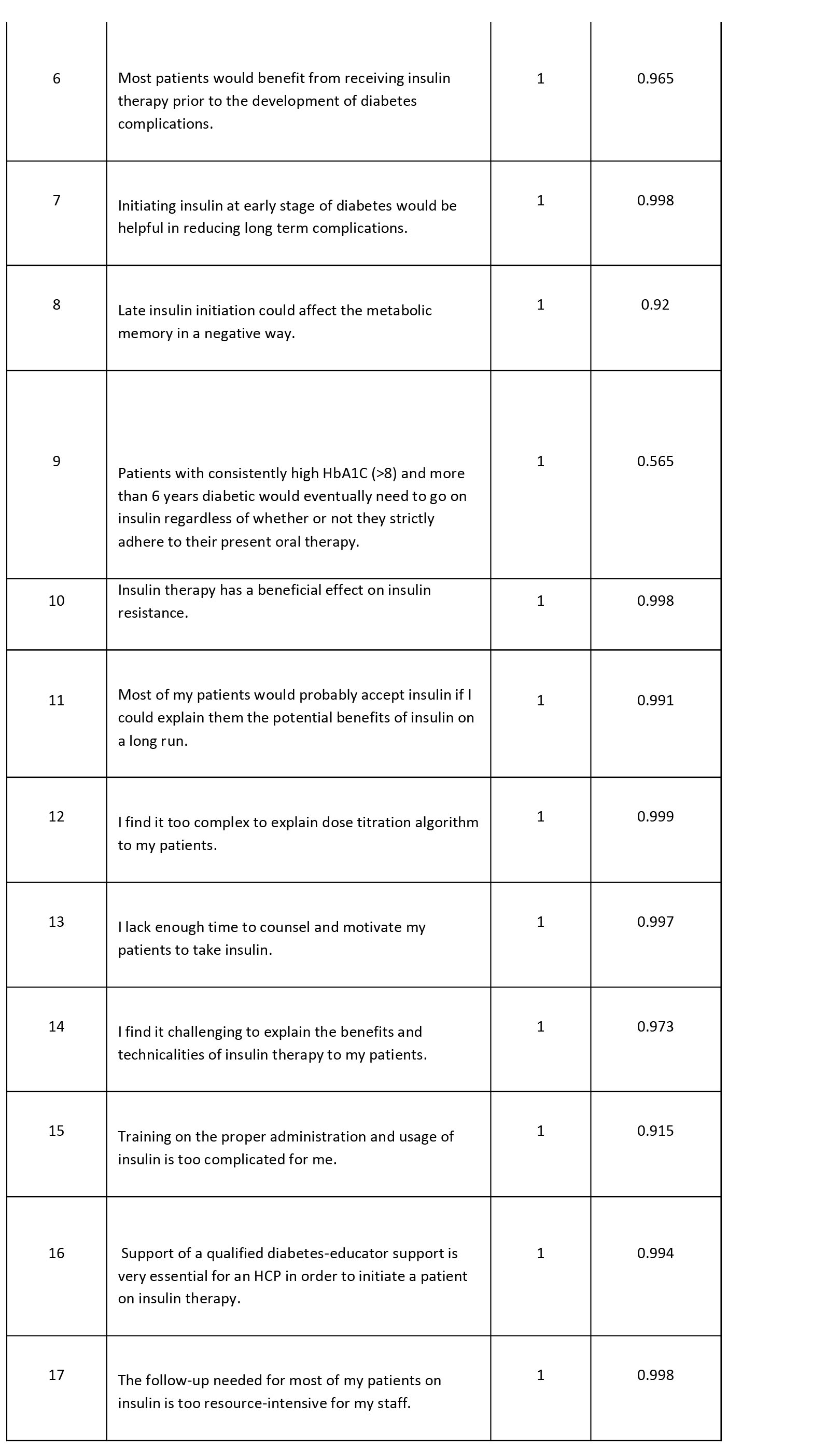
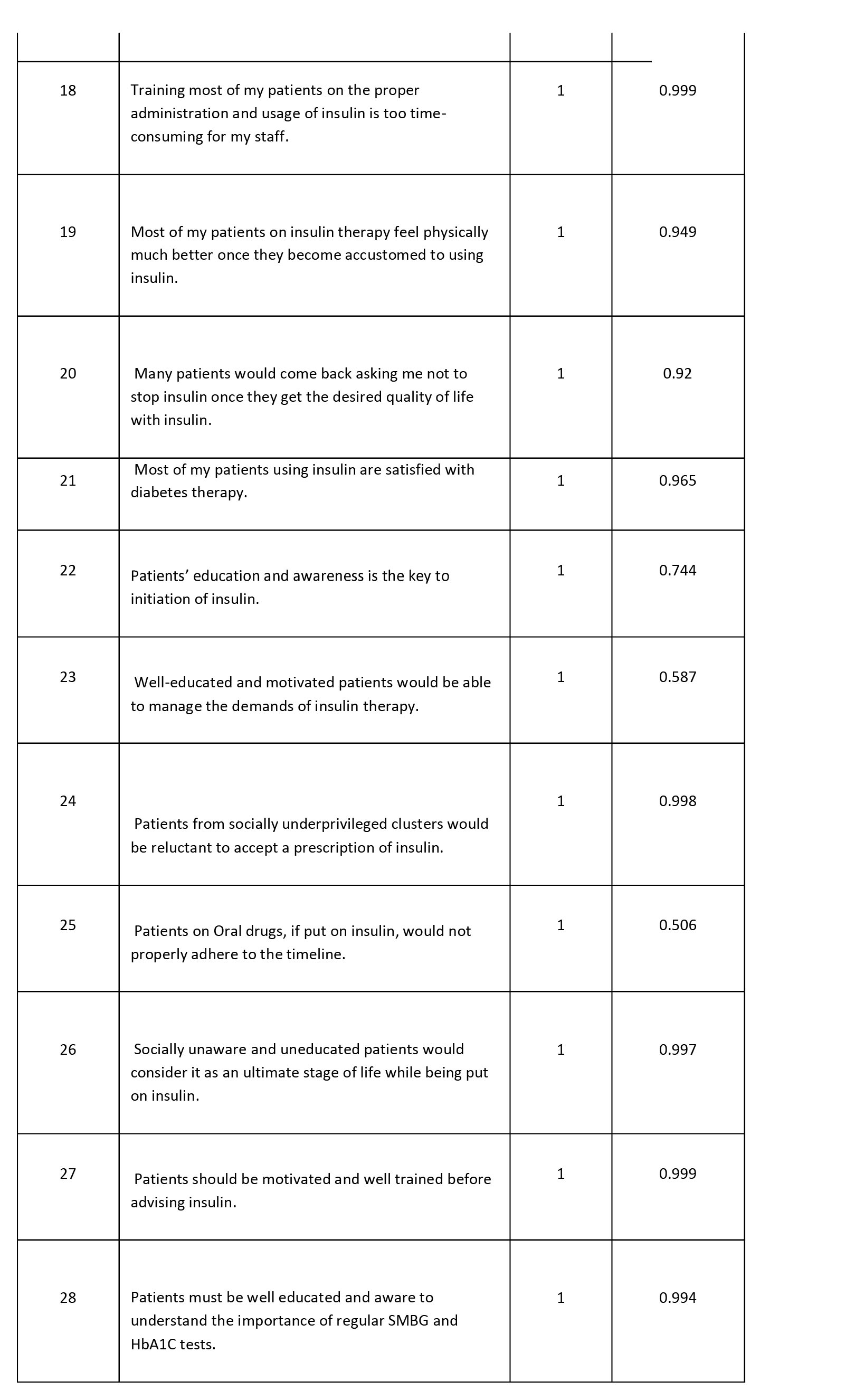
Interpretation of Test Results:
All the 28 items (variables) have ‘fairly high’ Extraction Communality values (≥0.5), indicating that each of these variables has a significant contribution towards a factor, and will be considered for further analysis. Thus NO variable is likely to be a target for elimination.
Rotated Component Matrixa
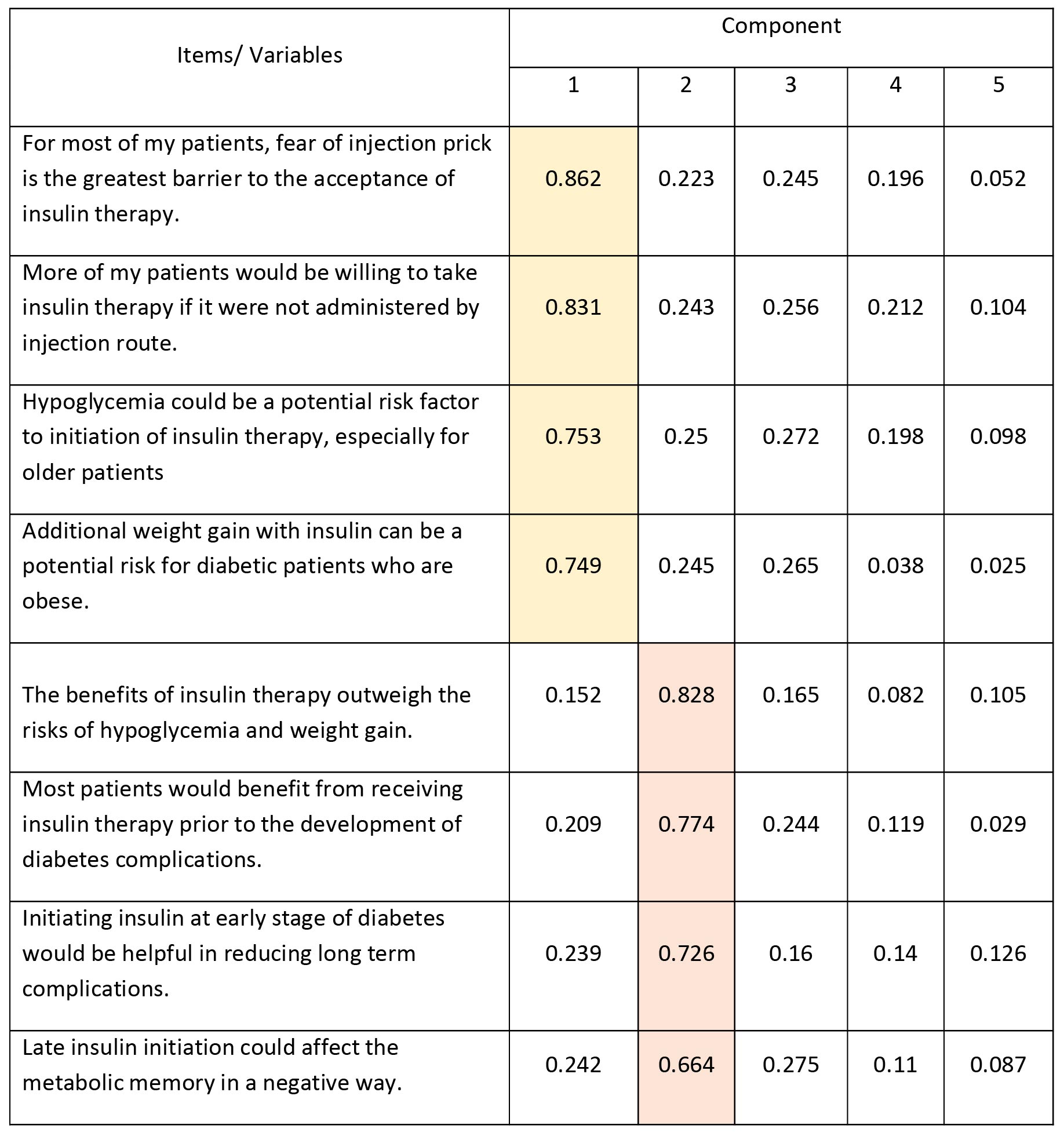
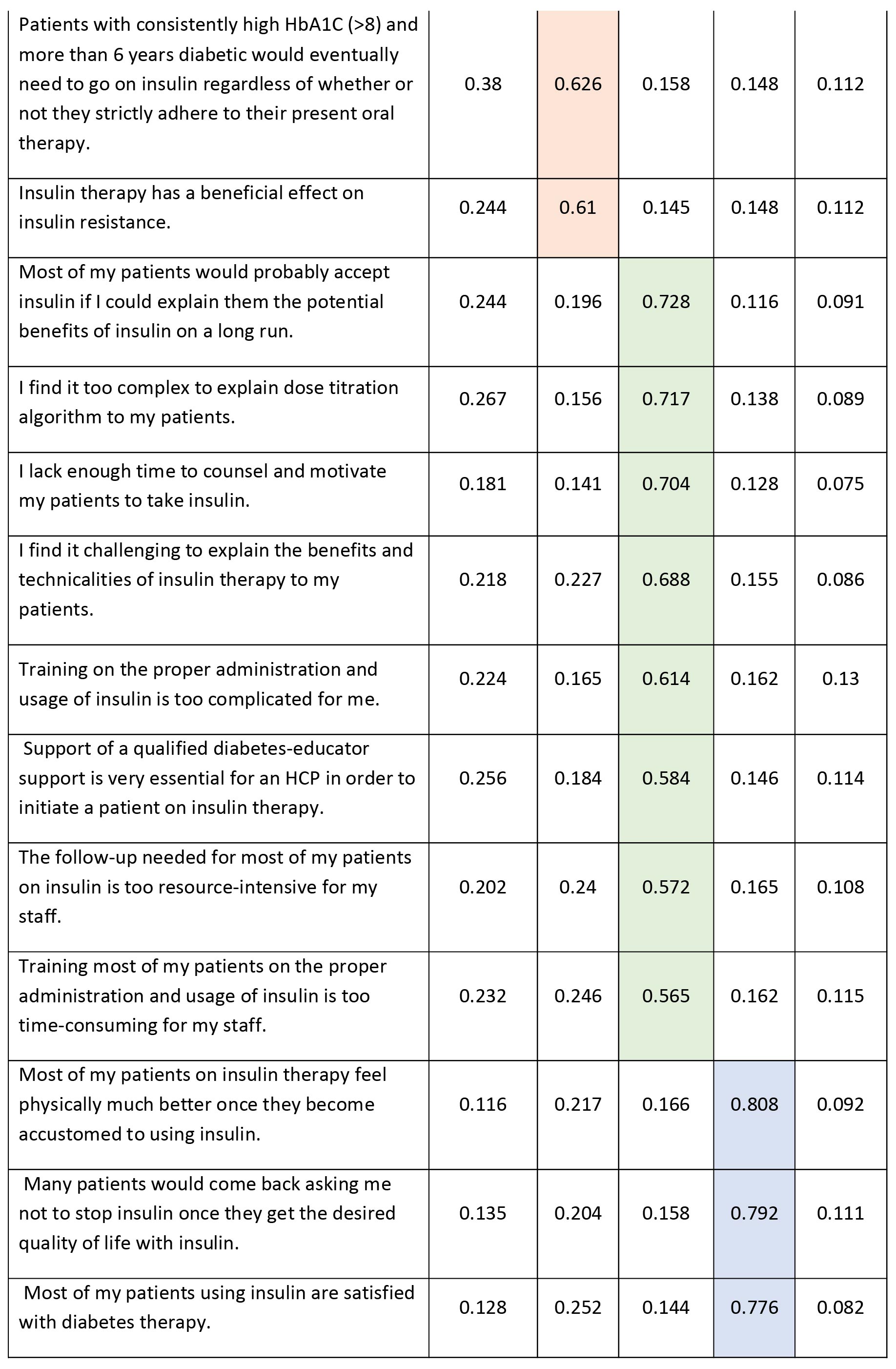
Extraction Method: Principal Component Analysis.
Rotation Method: Varimax with Kaiser Normalization.
a. Rotation converged in 6 iterations.
The above Principal Component Analysis generates 5 components, and outputs the loading values under each component. Based on the given values, we can club the items having highest factor loading values (cut-off ≥ 0.5) under one Component/ Factor. This way we have 5 Factors with us. They can be represented as:
FF: Fear Factors
CON: Clinical Conviction in early insulin initiation
CC: Capacity and Competency of HCP to educate and motivate patients.
QOL: Quality of Life and Patient Satisfaction.
EMA: Education, awareness and motivation among the patients.
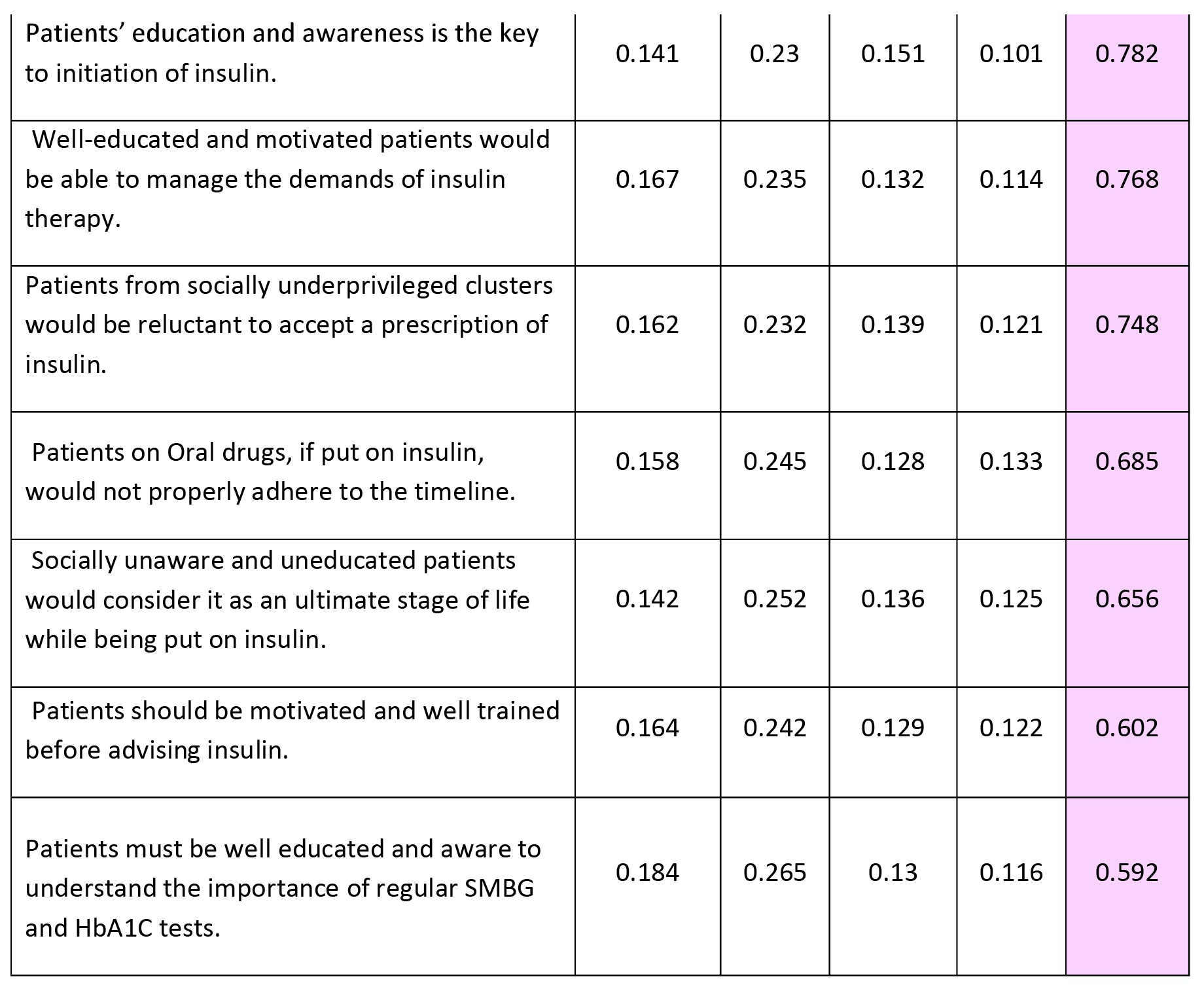
Interpretation:
- The alpha coefficient of 0.725 (≥ cut-off value=0.70) for the 4 items in the FF factor suggests that there is relatively high degree of internal consistency amongst the items.
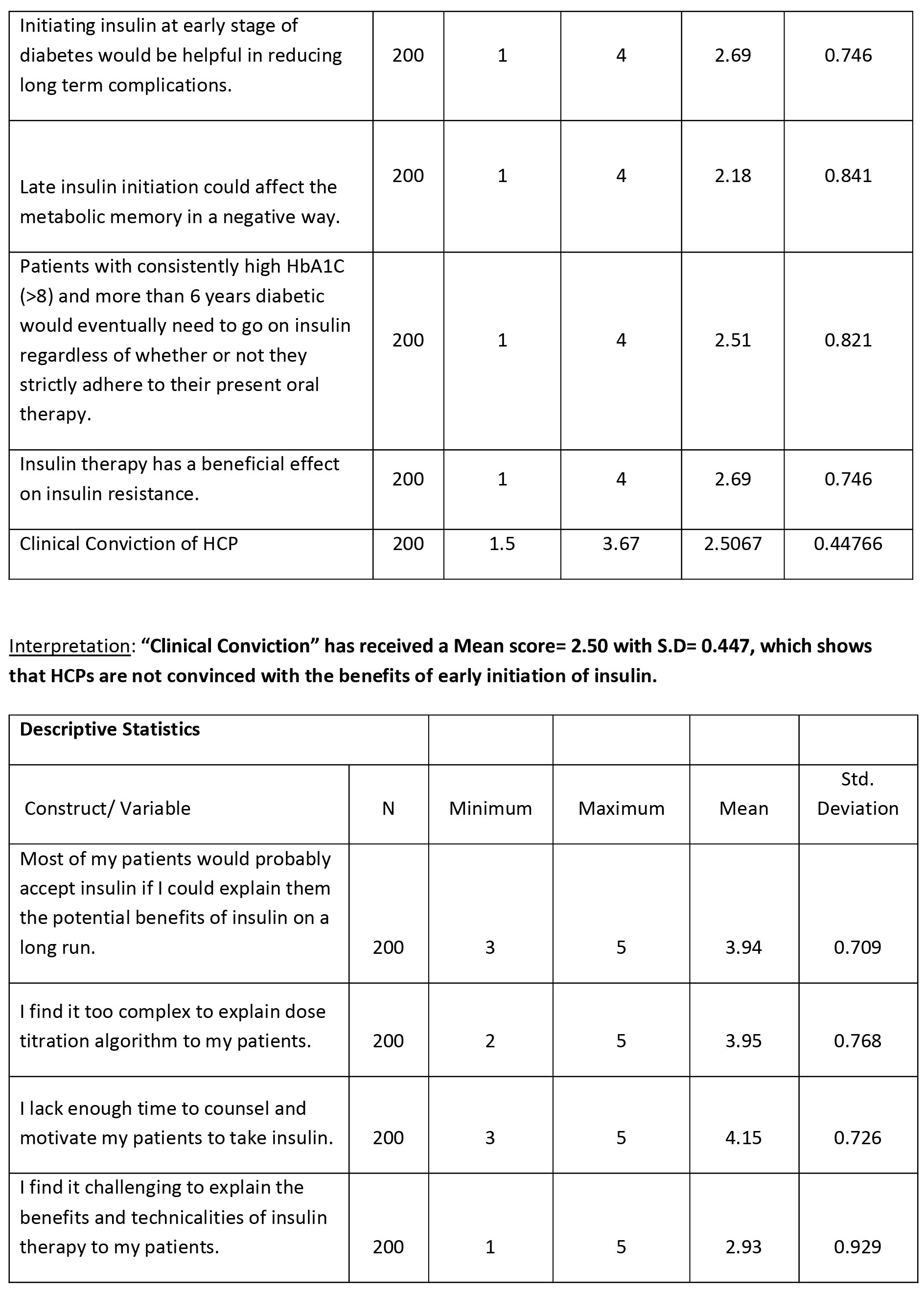
- The alpha coefficient of 0.856 (≥ cut-off value=0.70) for the 6 items in the CON factor suggests that there is relatively high degree of internal consistency amongst the items.
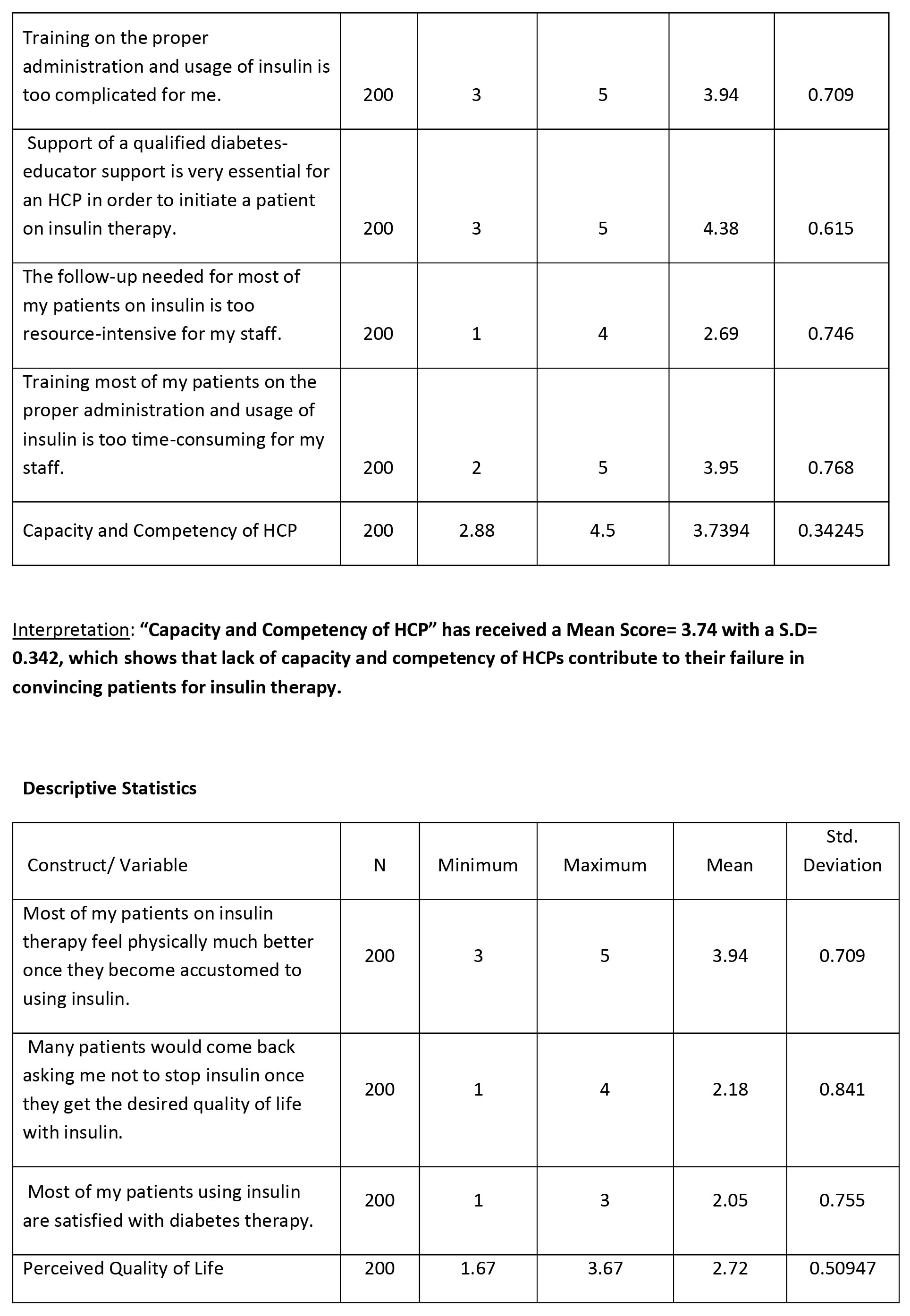
- The alpha coefficient of 0.902 (≥ cut-off value=0.70) for the 8 items in the CC factor suggests that there is relatively high degree of internal consistency amongst the items.
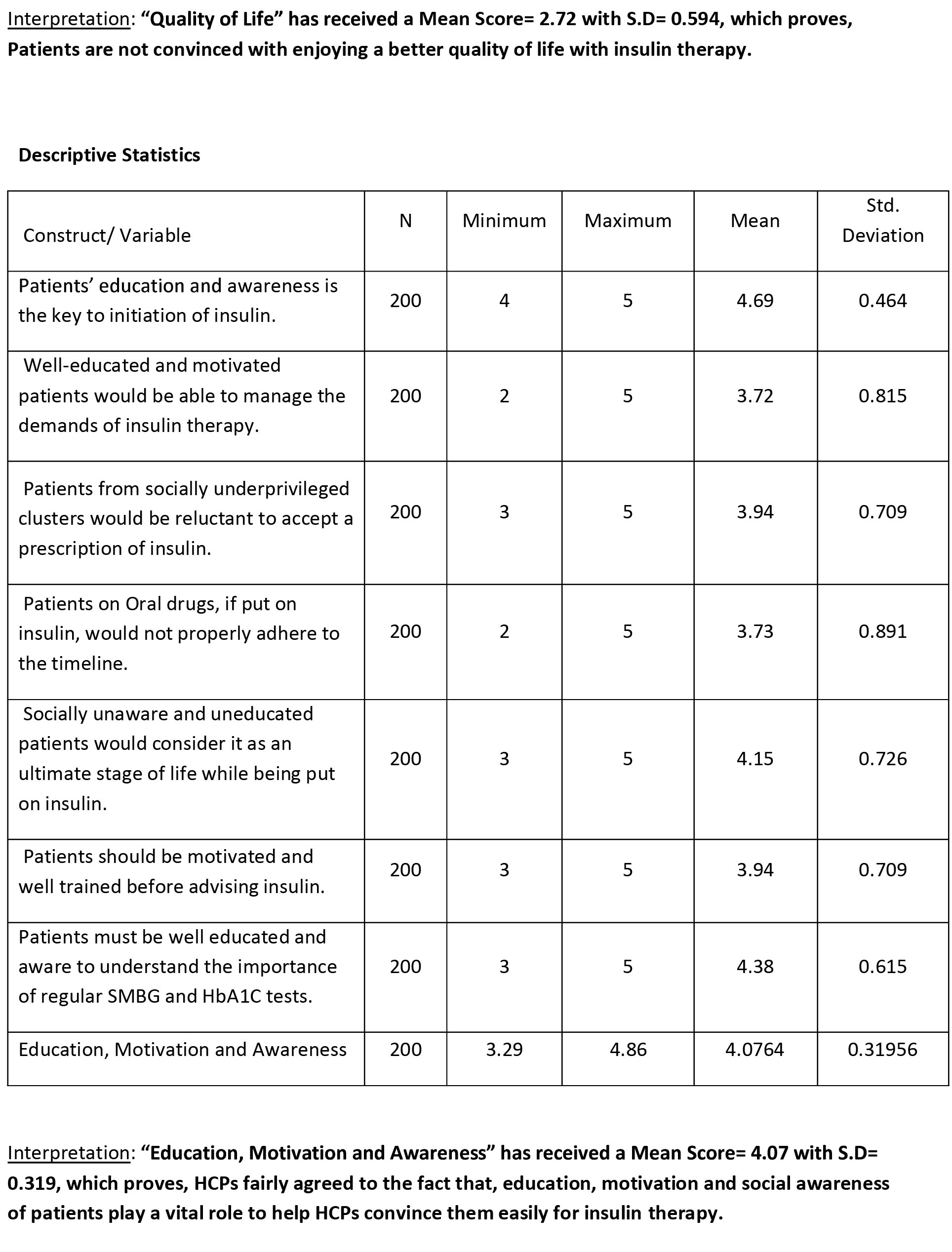
- The alpha coefficient of 0.714 (≥ cut-off value=0.70) for the 3 items in the QOL factor suggests that there is relatively high degree of internal consistency amongst the items.
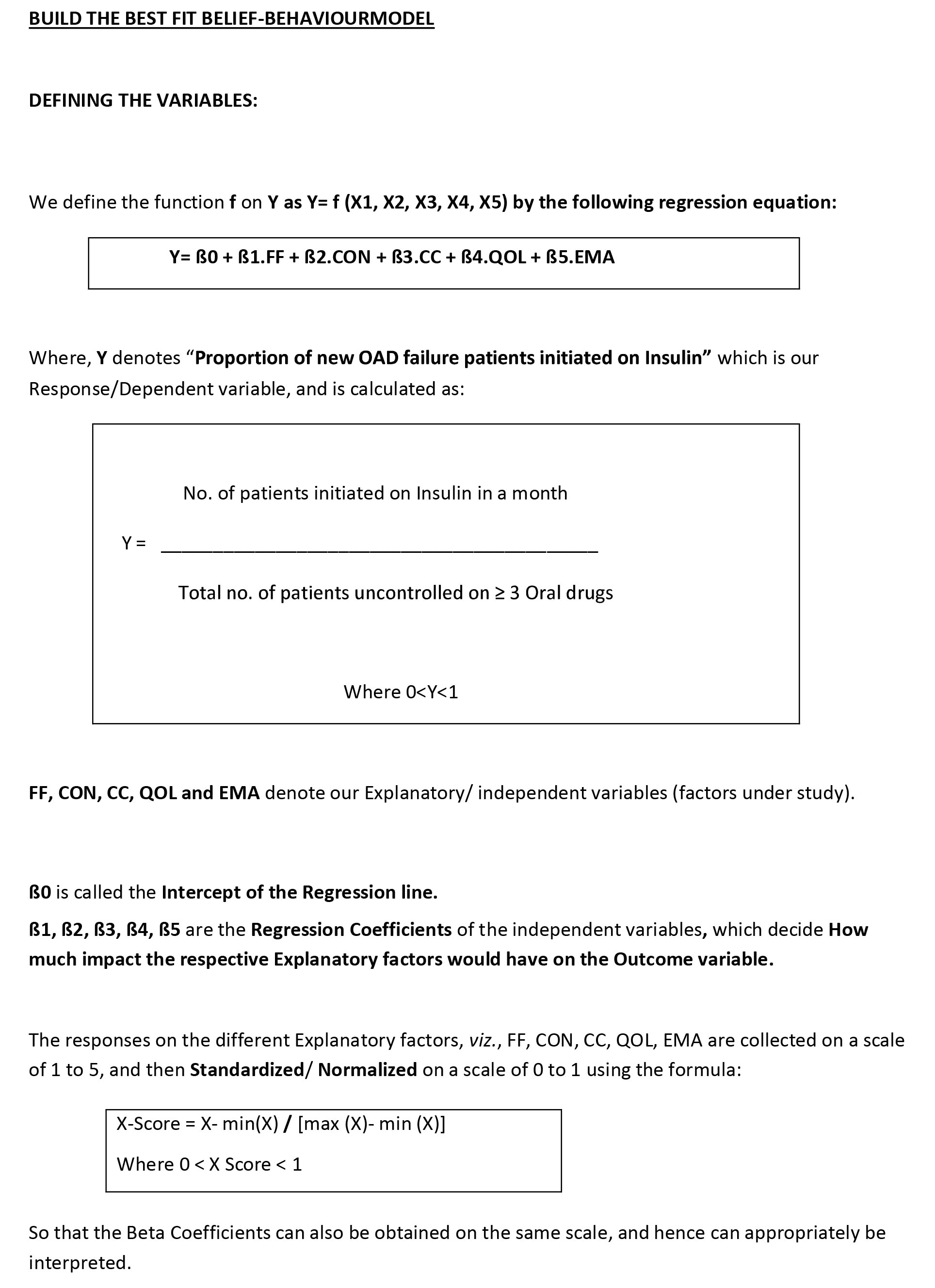
- The alpha coefficient of 0.887 (≥ cut-off value=0.70) for the 7 items in the EMA factor suggests that there is relatively high degree of internal consistency amongst the items.
Where,
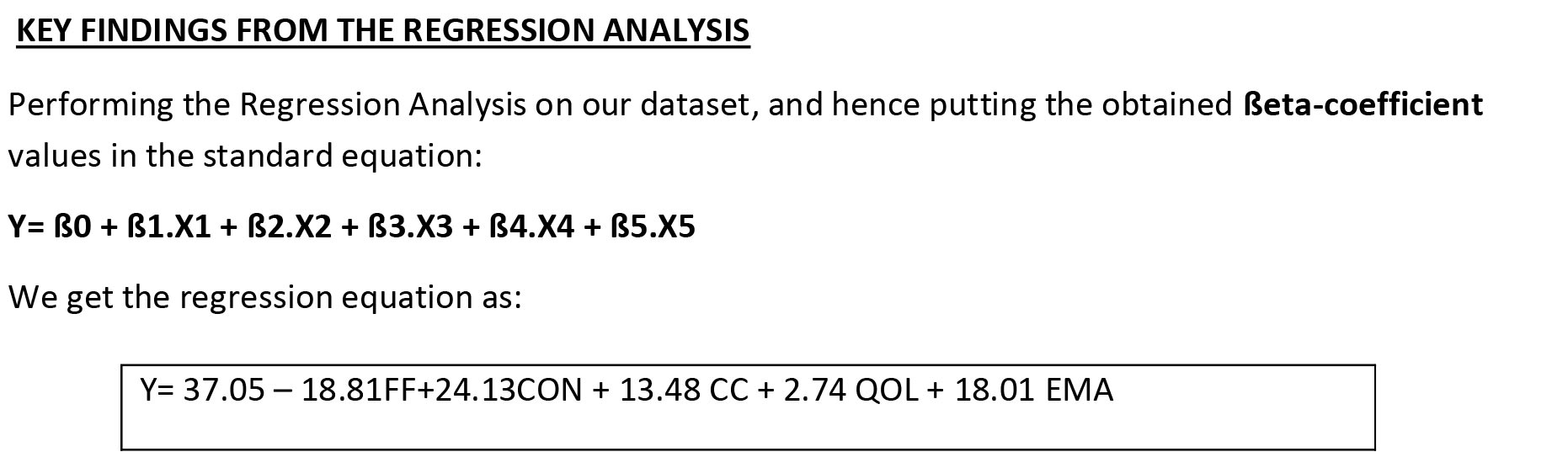
β0= 37.05 is called the Intercept of the above straight line, which is the value of the Response variable when all the Explanatory variables are kept at Zero. All the Explanatory variables held at Zero do not have any managerial implication, and hence β0 has no relevance in our study.
❖ β1= -18.81 is the Regression Coefficient of FF on Y, which implies, for every 1 % decrease of Fear Factor of HCP, proportion of insulin initiation is likely to increase by 18.81%, all other variables kept at the same level.
❖ β2= 24.13 implies that for every 1 % increase in Clinical Conviction of HCP, proportion of insulin initiation is likely to increase by 24.13 %, all other variables kept at the same level.
❖ β3= 13.48 implies that for every 1 % increase in Capacity and Competency of a HCP, proportion of insulin initiation is likely to increase by 13.48 %, all other variables kept at the same level.
❖ β4= 2.74 implies that for every 1% increase in Perceived value of Quality of life and well-being of a patient, proportion of insulin initiation by the respective HCP is likely to increase by 2.74 %, all other variables kept at the same level.
❖ β5= 18.01 implies that for every 1% increase in Education, Motivation and Awareness level proportion of insulin initiation is likely to increase by 18.01 %, all other variables kept at the same level.
At 5% Significance level, the P-Values of the βeta-coefficients of the Explanatory factors, [FF (p=0.00206), CON (p=0.00185), CC (p=0.021), and EMA (p=0.00102)] are all≤ 0.05 (statistically significant), which means that we can rule out a true Zero value for these ßeta-coefficients; or in other words we can say that, these factors have a significant impact on our Response variable, i.e, these factors are important in explaining the variation in Proportion of new initiation.
On the contrary, the ßeta-coefficient of the factor QOL(p=0.0627) having P-value > 0.05 (statistically non-significant ) can have Zero as a true admissible value in the 95% C.I, or in other words, QOL does not have a significant impact on our Response variable, implying that this factor is not important in explaining the variation in Proportion of new initiation.
For this particular model,
We observe that the value of R-square= 0.86 (approx.), implying that this is a highly reliable model which is able to explain 86 % variation in Proportion of new initiation.
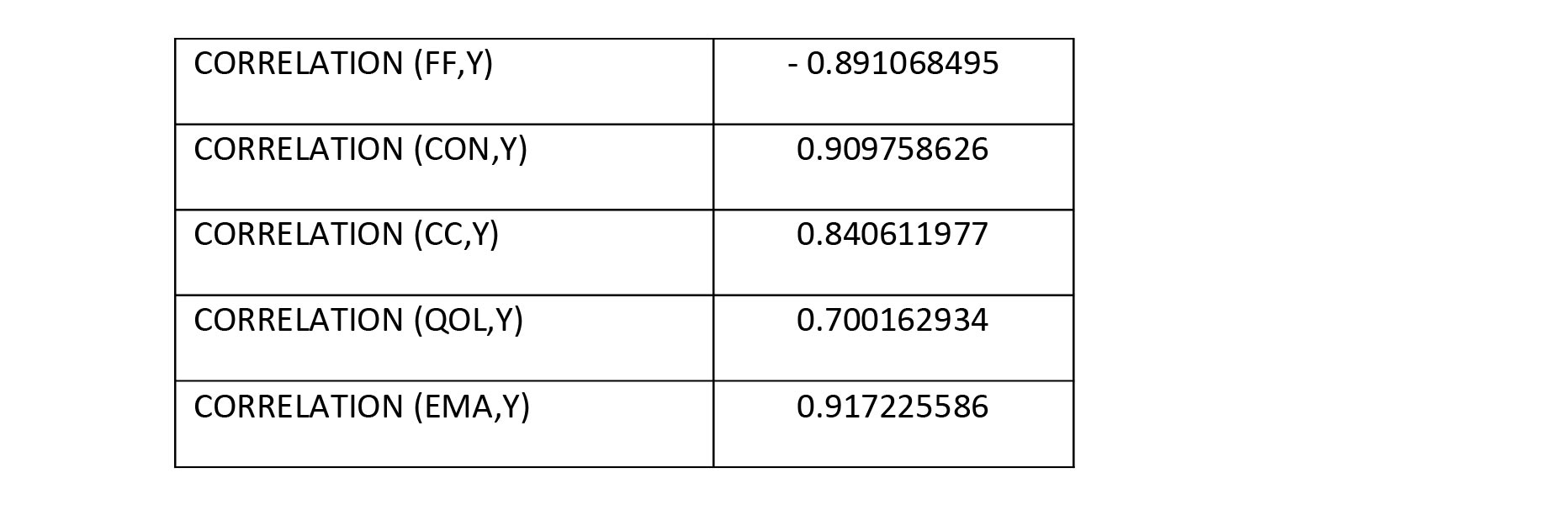
Also we derive the pairwise Correlation coefficients of each of the Explanatory factors and the
Response variable, and observe that, all the Explanatory factors have a very strong Positive/
Negative correlation, or in words all of them bear a very high degree of association with the
Response (Dependent) variable.
KEY CONCLUSIONS
❖ The Beta-Coefficient for Clinical Conviction suggests that, HCPs must have a high degree of conviction on the benefits of early insulin initiation on a long run for better treatment satisfaction and attain optimal glycemic control. In this regard it is suggested that HCPs must upgrade their knowledge on the various advancements in the field of diabetes by repeated exposures to more no. of CMEs on insulin initiation and therapy management. This will help them to gain confidence in initiating insulin.
❖ HCPs must upgrade their set-up to have adequate capacity in terms of supporting patients with hands-on training on insulin usage, its storage and administration.
❖ HCPs must be in a position to counsel the patients on the potential benefits of insulin therapy on a long run, and thus remove the fear of prick from their mind. They should also spend adequate time motivating them as to how insulin therapy would give them a better quality of life and well-being. The patients must be guided on how they can avoid an event of hypoglycemia by timely intake of food. Also a diabetic patient should be strictly advised to be on a customized diet for body-weight management. A diabetes educator support will come handy in regard to the above two propositions.
❖ As education and social awareness is an important factor, it is advised that HCPs must organize ‘Patients Education and Empowerment programs’ periodically to continuously educate and motivate diabetic patients on the various aspects of diabetes and their reinforcement, so that they can happily accept a prescription of insulin.
❖ ‘Perceived Quality of Life’ by a patient does not have a significant impact on the initiation of insulin therapy by an HCP, although HCPs must make it a point to make patients perceive better QOL with insulin therapy while counseling and motivating them.
❖ HCPs should be well versed with the titration algorithm of insulin depending on the ever changing glycemic profile of a patient. They should try and keep it simple for the patient, and try to initiate an insulin which is easy to titrate without any complexity in it (preferably a Basal insulin).
❖ Patients should also be explained the importance of regular Self-Monitoring of blood glucose by keeping a support of glucometer at home, and also to get their HbA1C tested from time to time.
REFERNCES:
Jindal, S., &Kalra, S. (2020). Developing a definition for Oral Antidiabetic Drug (OAD) Failure. JPMA, 2019.
https://care.diabetesjournals.org/content/42/3/476#ref-1
https://care.diabetesjournals.org/content/42/3/476#ref-1
https://care.diabetesjournals.org/content/42/3/476#ref-2
https://care.diabetesjournals.org/content/42/3/476#ref-6
Hayes, R. P., Fitzgerald, J. T., &Jacober, S. J. (2008). Primary care physician beliefs about insulin initiation in patients with type 2 diabetes. International Journal of Clinical Practice, 62(6), 860-868.
Chalmers, J., & Cooper, M. E. (2008). UKPDS and the legacy effect.
Monnier, L., Lapinski, H., & Colette, C. (2003). Contributions of fasting and postprandial plasma glucose increments to the overall hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA1c. Diabetes care, 26(3), 881-885.
Das, A. K., Mithal, A., Kumar, K. M. P., Unnikrishnan, A. G., Kalra, S., Thacker, H., & Joshi, S. (2020). Rationale, study design and methodology of the LANDMARC trial: a 3‐year, pan‐India, prospective, longitudinal study to assess management and real‐world outcomes of diabetes mellitus. Diabetic Medicine, 37(5), 885-892.
Ellis, K., Mulnier, H., & Forbes, A. (2018). Perceptions of insulin use in type 2 diabetes in primary care: a thematic synthesis. BMC family practice, 19(1), 1-21.
Mohan, V., Shah, S. N., Joshi, S. R., Seshiah, V., Sahay, B. K., Banerjee, S., ... &DiabCare India 2011 Study Group. (2014). Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: results from the DiabCare India 2011 Study. Indian journal of endocrinology and metabolism, 18(3), 370.
Holman, R. R. (2006). Long-term efficacy of sulfonylureas: a United Kingdom Prospective Diabetes Study perspective. Metabolism, 55, S2-S5.
