Subscribe now to get notified about IU Jharkhand journal updates!
Knowledge, Attitude and Practice of Medical Practitioners towards Standards of Tuberculosis Care through Private Public Partnership working in neighbouring districts of Kerala and Karnataka
Abstract :
More than 60% of the TB patients approach the private practitioners in India. To achieve control over rapid rise in prevalence of TB in India, involving the private practitioners as key stakeholders should remain the main objective of the Government of India. Aim: To assess and discuss the involvement of private practitioners in the diagnosis, treatment and control of TB in the neighboring districts of Kerala and Karnataka. Objectives: To assess the Knowledge, Attitude and Practices of Medical Practitioners towards Standards of Tuberculosis Care (RNTCP Programme) through Private Public Partnership working in neighbouring Border Districts of Kerala and Karnataka. Methods: A Cross-sectional Study by using a self-administered questionnaire was conducted among 100 Private and Government practitioners. The study questionnaire was sent to 100 doctors out of which 94 practitioners participated. Data was collected and analysed. Among the 94participants, 90 (95.74%) were prescribing anti TB drugs. 04 (04.25%) reported as not prescribing Anti TB Drugs. 46/90 (51.11%) were giving prescription for four standard drugs with appropriate dosages and duration. 14/90 (15.55%) practitioners were not following the anti TB regimen advised by national programme .30/90 (33.33%) practitioners did not answer the questions related to prescribing practices adopted by them. 68/90 (75.55%) practitioners anti TB treatment was given for 6 months. 06/90 (06.66%) practitioners answered as 1 to 05 months. 16/90 (17.77%) practitioners answered as 07 to 08 months. The Knowledge, Attitude and Practices of Medical Practitioners working in border districts of Kerala and Karnataka towards Standards of Tuberculosis Care was reasonably good. Even though patients belonged to separate states, notification of cases to Government of India through proper channel was good among the medical practitioners. Limitation of this study was smaller sample size and at two border district only.
Keywords :
Tuberculosis, TB care, notification, border districts, treatment outcome.1.Introduction
If we look at the Annual global incidence of Tuberculosis, one fourth of it occurs in India. (1) To end the global TB epidemic there should be rapid implementation of active National TB control Programme in India. Intervening and acceleration for TB prevention and care in India are important to end the global TB epidemic."High-quality health systems (HQSS)" in the persistent advancement Goals era" report published by Lancet stressed for a revolution (2). The report envisages that implementing anti TB programmes without assuring a minimal degree of quality is ineffective, wasteful, and unethical. It required high-quality health systems that standardizes and provides health
care in every aspect of the anti TB Programme consistently delivers the care to improve or maintain health which should be valued and trusted by all people, and by responding to changing population needs.(2) Providing the detailed death analysis of TB patients globally states that out of 946,003 TB deaths amenable to healthcare, 469,956 (50%) deaths were due to poor quality TB care and the remaining 476,047 deaths were due to non-utilization of healthcare services.(2) The report also suggested that high-quality health systems could have prevented 900,000 TB deaths each year.(2) It means that we could prevent TB deaths if all the existing health care facilities are better utilized. Deaths due to TB were estimated to be 1.6 millions in 2017. The death rate due to TB had overtaken the death rate of HIV/AIDS.(3) The lower HIV/AIDS mortality was due to the effects of massive global investment in better diagnosis and antiretroviral therapy. (3)Comparison of TB cases lost in the cascade of health care system instituted in its control, among the countries globally contributing to the death rate, it was found that in South Africa the TB cases were lost in 47% of TB cases 15%) at test access, 13% during diagnosis period, 12% while starting treatment and 17% reaching at completion of successful treatment), (4). Whereas In India 40% of the patients were lost before they were diagnosed. (5) In China the prevalence rate dropped from 215 in 1990 to 108 in 2010 but the undiagnosed patients remained high (6). To overcome the bottlenecks in th cascade of anti TB control Programme, researchers have introduced method of standardized patients (SPs) who help to measure the quality of TB diagnosis and treatment in multiple settings. In this SP method, a team of trained local people were involved who themselves present as patients at a surprise movement to the health care providers with the same set of scripted symptoms (in this case, typical symptoms of TB). (7) Development of resistance to the primary line of TB treatment resulting in drug Resistant variants of Mycobacterium Tuberculosis (DR-TB) remains the world's most significant threat to global Health and multiplying the death rate. (8) Insufficient facilities to help the early diagnosis of DR-TB resulted in 160,684 out of 558,000 population were found tohave developed DR-TB each year,were diagnosed and among them only 139,114 (25%) were started on appropriate treatment; poor quality care was rampant in the field. (9) This in turn was reflected on the final outcome of 65% of the TB cases treated all over the world. "Patient centered" TB treatment were the words recently introduced in the vocabulary of TB Control Programmes with actual practices of safety, equity, and effectiveness which are all quality domains are to be introduced wherever there were urgent needs to improve DR-TB treatment. (10) Even though there are no reported evidences ofregular assessments of quality of DR-TB care, it was concluded that earlier efforts were focused on patients already under TB treatment for drug-susceptible TB. It was a fact that DR-TB occurs by primary transmission especially among those people who live with the patients receiving anti TB treatment. (11)This fact was one of the reasons theTB care quality has been significantly understudied in the field of DR-TB. (12) In India studies conducted with mixed-methods have shown that the quality of life measures among the people of DR-TB was low more so in their physical and psychological
domains. (13) Many researchers are of the view that TB problem in India is very idiosyncratic with variegated quality often different from global standards. (14) The TB- care quality among the patients in both the private and public sectors was astonishingly diverse across the clinics, cities and states. (15) Hence special attention was required especially in India where RD-TB is a major problem and pharmacies dispense anti TB drugs without prescription. (16) According to WHO (World Health Organization) reports in 2018, 64% out of accounted 10 million TB cases diagnosed and treated all over the world 3.6 million cases are left out without care or or no care at all. (17) On September 2018 during the first United Nations High-Level Meeting on the Fight to End TB (UN HLM), there was greater emphasis on improving TB case detection, TB prevention, and ensuring timely care for all people with active TB disease. (17)In coordination with the countries adding major contribution to the TB problem, the final destination of the UN HLM was to speed up the progress of elimination of TB as a burden of public health challenge. (18) The targets aimed to achieve this goal was towards treatmentofpatients with drug sensitive TB, drug resistant TB (DR-TB), pediatric case diagnosis, preventive TB therapy among the people who are in contact with confirmed TB cases and those populations who are living with AIDS/HIV. Assessing the quality of LIfe (QOL) during the TB cases management a scale could be used in TB research programmes such as Short Form 36 (SF-36), (19). This gives scores across 8 domains such as Role Physical, Physical Functioning, General Health, Bodily Pain, Social functioning, Vitality, Emotional, and Mental Health, and two summary scores - Physical Component Score and Mental Component Score. These assessments are necessary in TB Infection prevention control (TB-IPC). (20, 21) One third of the AIDS related deaths occur due to TB in India or elsewhere in the World. (22) out of nearly 1.6 million people who died from TB included 3 Lakh people with AIDS. (23) The main reason for such an occurrence was due to failure to enrol for TB prevention therapy in patients diagnosed with AIDS; only 36% of newly enrolled patients were included in TB prevention therapy (23). World Health Assembly approved "End TB Strategy" in 2014;with an ambitious target to end the worldwide TB epidemic by 2035. (24) United Nations Political Declaration in 2016, on Ending AIDS targeted to reduction in 75% of AIDS related to TB origin by 2020. (25) WHO coined "End TB strategy" targeted to initiate TB therapy in 90% of TB positive cases as well as high risk TB cases by 2030. (26)In spite of these decisions by the world bodies there is a slow progress and quality gaps in TB and HIV services in all the countries. The reasons analysed for such a situation could be due to the following factors such as with suboptimal utilization of tests such as urine lipoarabinomannan (LAM) for TB diagnosis in HIV patients, lack of Xpert a molecular diagnostic platform and MTB/RIF, poor access to ideal TB prevention and treatment regimens, infrastructure, anti TB drugs supply, diagnostics and BCG vaccines, and information systems challenges, as a few examples. (27)In India cascade analyses at National-level TB care have shown that large numbers of TB cases experienced poor outcome at all critical points in health system engagement, which highlighted foundational problems in the quality of TB care Programmes. (28, 29) Such analyses may help in quantifying the gaps in TB care delivery but fail to highlight as to why patients fall through these cracks which is necessary for improving interventions to upgrade outcomes in TB programs. (30) To rectify such gaps requires
interventions at different levels: Large-scale public education, increased access to health facilities, initiatives in the private sector, integration of new diagnostic and monitoring technologies, and interventions to address patients' psychosocial needs. (31, 32) Globally the estimated number of children those died of TB was 205,000 in 2018; including 32,000 (16%) of HIV children (mortality rate of 18.3%). (33)96% of the children among them were not treated and 80% of these children could not survive beyond five years. (34) In young children diagnosis of TB is difficult (especially children with HIV) because there is overlap of symptoms and signs with non-TB Pneumonias resulting in under-reporting of TB-related child deaths. Microbiological diagnosis is also difficult and challenging in children. (35) The TB diagnosis and reporting gap among the children was found to be as high as among all age groups touching he 33% mark globally, and remains disproportionately high at 63.3% in children under 5 years of age. (36)87% of the global burden of Child TB cases was found among the 8 countries alone which includes India, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa. Whereas the TB preventive treatment (TPT) figures among these countries was found to be varying from 6% (Indonesia), 14% (Nigeria) and 34% in India;with the exception of South Africa reporting 59-65% TPT coverage in children. (35, 37)In low Socio-economic countries the role of community pharmacies is limited to dispensing and retailing medicines (top 3 countries accounting to global gap; India, Nigeria and Indonesia have large chains of private pharmacies). But their potential if could be utilized in the filling prescriptions for anti-TB medication and dispensing, the fight against TB could be so much greater, as the extensive utilization and accessibility by communities. They could be used as an diagnostic oppurtunity as in high burden countries where patients experiencing the non-specific symptoms of TB (typically a prolonged cough) often seek care, initially at a private pharmacy. (38) Pharmacies could take a role of Directly Observed Therapy (DOTS), a cornerstone of the Stop TB Strategy. (39) This type of involvement of pharmacies in the National Programme of Control of TB has been recognized globally and falls into the engagement of private providers within national TB programmes (public private mix- PPM). (40)In 2011 WHO and International Pharmaceutical Federation (FIP) suggested that the National TB programmes and pharmacy services in the countries could be used to implement plans to fight against TB. (41) But not many countries have utilized the urge of these two organizations. 10% of the 1.7 billion Latent TB (LTBI) patients (one quarter of world population) will progress to active TB (170 million). (42) To reduce the reservoir of individuals who are LTBI the WHO urged for patient-centered care and increased provision of preventive treatment as an End TB strategy. (43) United Nations during its first High Level Meeting on TB (UNHLM-TB), in 2018, announced with a commitment to end TB by 2035 and planned to target providing 30 million people with preventive treatment for LTBI by 2022. As a consequence of the mismanagement of TB care programmes an an estimated 500,000 new cases of rifampicin- resistant TB (RR-TB) out of them 78% were multi-drug resistant TB (MDR-TB) cases. (44) The objective of End TB Strategy was to provide TB patients with high-quality care, with his human rights being central to its design and delivery of TB services.(44)There have been big losses of patients for follow-up of patients during the points of the TB care cascade, where 50% of patients are diagnosed and treated adequately. Healthcare providers are only correctly managing 21-50% of TB patients, and patients often visit multiple providers before receiving a correct diagnosis. (45) Tuberculosis (TB) accounts for one of the top ten causes of death globally. Since 2011 it has surpassed HIV/AIDS, accounting for 1.2 million deaths among HIV negative with TB people. (46) Another deaths occur in 0.25 million people with HIV people with TB. (46)The present target of reducing 75% of TB mortality by 2025 is very an ambitious milestone (TB mortality in HIV negative patients is falling by 3% / year. (46)Cure rates among the TB patients was 95% and more in developed countries, thanks to the prompt supply of effective anti- TB drugs and firmly assured adherence to therapy. (47) The case fatality ratio (estimated mortality/estimated incidence) in high-income countries is 5% but it is around 20% in high-burden countries. (46) The countries with high TB burden contributing to two thirds of the disease burden are India-27%, China-9%, Indonesia-8%, Philippines-6%, Pakistan-5%, Nigeria-4%, Bangladesh-4% and South Africa-3%. (46) In India an effort should be made to reduce the disease burden and deaths due to TB which will be crucial in achieving these ambitious targets. UN-HLM (High level meeting) followed by highlights of Lancet Commission have delved into the critical importance of improving the quality of TB care to achieve all the targets of treatment and prevention of mortality and morbidity. Most of the high TB burden countries have focused and expanded the coverage of directly observed therapy (DOTS), short course (s-DOTS) over the last quarter century but few have attempted to evaluate or address the quality of TB care offered. (47) High quality TB care is defined as care that is patient-centric, matches the international standards and made available in time, safely, effectively and in an equitable manner. (48) To achieve the UN HLM targets, delivering high quality care must be a central focus across the health system, but especially at the facility level. (49) The quality of TB care appears like, relies on who was defining it. Always the Healthcare must adhere to evidence-based guidelines, present nominal risks and short delays for service users, and they must be available equally to all, regardless of factors like race, gender, geography, and socioeconomic status. It calls for healthcare that is people- Centric, and takes into account the preferences and aspirations of individual service users and their communities.(50) Review of literature on Private Health care providers in low- and middle-income countries showed that they are an important source of healthcare for all Socio-economic strata. The less-poor people go to formal and qualified health providers, while the poor go to informal and unqualified health providers. (51) These Private health providers account for 50-70% of health care, especially outpatient primary care and especially in urban areas. (51) These private health care providers are difficult to be approached by surveyors because of their large numbers, low case yield per provider, their minimal administrative capacities, and the fact that in many cases they operate on the borders of legality. Whereas the specialists and hospitals are fewer in number but are easier to be approached, they can take on more complex tasks and may often have relatively high case-loads, but they also tend to serve high socio-economic groups and are unlikely to be the first providers consulted. According to WHO 3 out of 10 million population who contacted TB in 2018 were totally "missed", i.e. they were not identified and informed notified by Government programmes. (52) Three countries - India, Indonesia and Nigeria - account for 46% of all missing people with TB, while a further 7 countries accounted for a further 34%.
The TB services were stalling even before the onset of the COVI-19 pandemic. There was little change in the 2020 Global TB report since the previous year. (53) The total number of population expired from TB in 2019 were 1.4 million. 3/10 millions of the people diagnosed with TB did not receive health care nor reported to the national authorities. It showed that the targets set by End TB, SDG and UN High Level TB meeting were grossly lagging. Out of the target of 30 million for TB preventive therapy by 2022, mere 6.3 million population had been treated between 2018 and 2019. A $6.5 billion pounds alone were raised during 2020 for the funding TB care out of the targeted $13 billion annually. (54)After and during Covid-19 pandemic The situation of TB care has worsened predictably.There was significant drop in the TB reporting all over the world. (55)Almost70% of TB healthcare workers and their supervisors havereported to have noticed a decreasedattending number of people approaching the health facilities for TB diagnosis. In India, 36% of TB patientsreported that the health centers they usually visit were found closed during CID-19 pandemic. The 2020 Global TB Report shows big reductions in TB notifications. The data showed 25-30% fall in notifications of TB cases especially from the three high burden countries such as India, Indonesia, the Philippines during the months of January to June 2020 when compared to the same 6-month period in the year 2019. As a part of 12th 5-year plan, the Government of India has approved the National Strategic Plan 2012-2017 that envisages "Universal access for quality diagnosis and treatment for all TB patients in the community." One of the key focus areas of the plan was to engage major part of private sector, and extend the Revised National Tuberculosis Control Programme (RNTCP) to patients diagnosed and treated by the private sector. (54) India has remained as a "High Burden Country" with the largest number of TB cases. In 2018 2.69 millionIndiancitizens got ill with TB and 0.45 milliondeaths occurred due to the disease (56, 57). In India NTEP (National TB Elimination Program) is being implemented which was previously called RNTCP (Revised National TB Control Program). This is a large public funded programme and caters to the people who uses the public health institutions for TB treatment. The program includes helping the people with diagnostic tests, treatment, follow-up and overall wellbeing of the patient. But, in India, 70% of the cases are being diagnosed from the Private sector which is said to be vast and unrecorded. Private sector also accounts for TB diagnosis and treatment where the quality and Standards for TB care in India (STCI) are not uniform. (58) In Kerala TB burden seems to be in a controlled situation especially with regards to drug resistant TB transmission rate. The state also has a well-developed private sector following reasonable standards in TB care. A published study reports that in two major cities of Kerala, 94% of the 124 participated TB practitioners prescribed a complete four-drug regime Isoniazide,Rifampicin, Ethambutol and Pyrizinamide for a minimum of 6 months to treat drug-sensitive TB. (59) People residing in Kasaragod district of Kerala is dependent on Mangaluru (Dakshina Kannada District of Karnataka) for Health care. The present study aims to assess and discuss the involvement of private practitioners in the diagnosis, treatment and control of TB in the neighbouring districts of Kerala and Karnataka.
Objectives of this study was to assessthe Knowledge, Attitude and Practices of Medical Practitioners towards Standards of Tuberculosis Care through Private Public Partnership working in northern Border Districts of Kerala and southern district of Karnataka
MATERIALS AND METHODS:
Study Design
Under the objective 1 a self administered questionnaire was used across a cross-section of Private Practitionersto assess the knowledge, attitude and practice of Medical practitioners in the border districts of Kerala and Karnataka. Under objective 2 for describing the outcomes of the treatments adopted analysis of the data collected from the self administered questionnaire.
Study Setting
RNTCP of India was implemented in the districts of Kasargod and Mangalore (Dakshina Kannada district) which are neighbouring districts of Kerala and Karnataka respectively. This project was implemented in close partnership with the District/State TB programme managers.
The Private medical practitioners of both these districts were given a self administered questionnaire and were asked fill up and return.
Inclusion Criteria: 1. In both the districts line listed qualified Private Practitioners who had the eligibility criteria mentioned below were involved for this study: (a) provide consultations to at least 10 patients per day, (b) willing to participate in the project, and (c) possessing an smart phone with android software and also willing to uutilize it for recording and reporting patient details. 2. All the engaged practitioners were appraised about the programme and the study, also to includee making use of the mobile application for presumptive TB patient referrals were included.
Exclusion Criteria: 1. Private practitioners who do not have modern medicine degree, unskilled health providers were excluded.
Study Period
The study was conducted between October 2019 and December 2020.
Study Population, Sampling, and Sample Size
For the quantitative component of the first study objective, all the Private Practitioners willing to join the study and be part of the project were enrolled for the study. For the second study objective necessary statistical methods were used.
Method: This study being a cross-sectional Study conducted in Kasaragod district of Kerala and Mangalore (Dakshina Kannada district of Karnataka) using a self-administered questionnaire, the study questionnaire was sent to 100 doctors to assess the attitudes and practices regarding Standards of TB Care and Private Public Partnership for TB control. Out of 100 doctors, only 94were willing to participate in the study.
Results were analysed with SPSS version 20 by assessing the frequency of data collected.
OBSERVATIONS AND RESULTS:
Knowledge and Attitude:
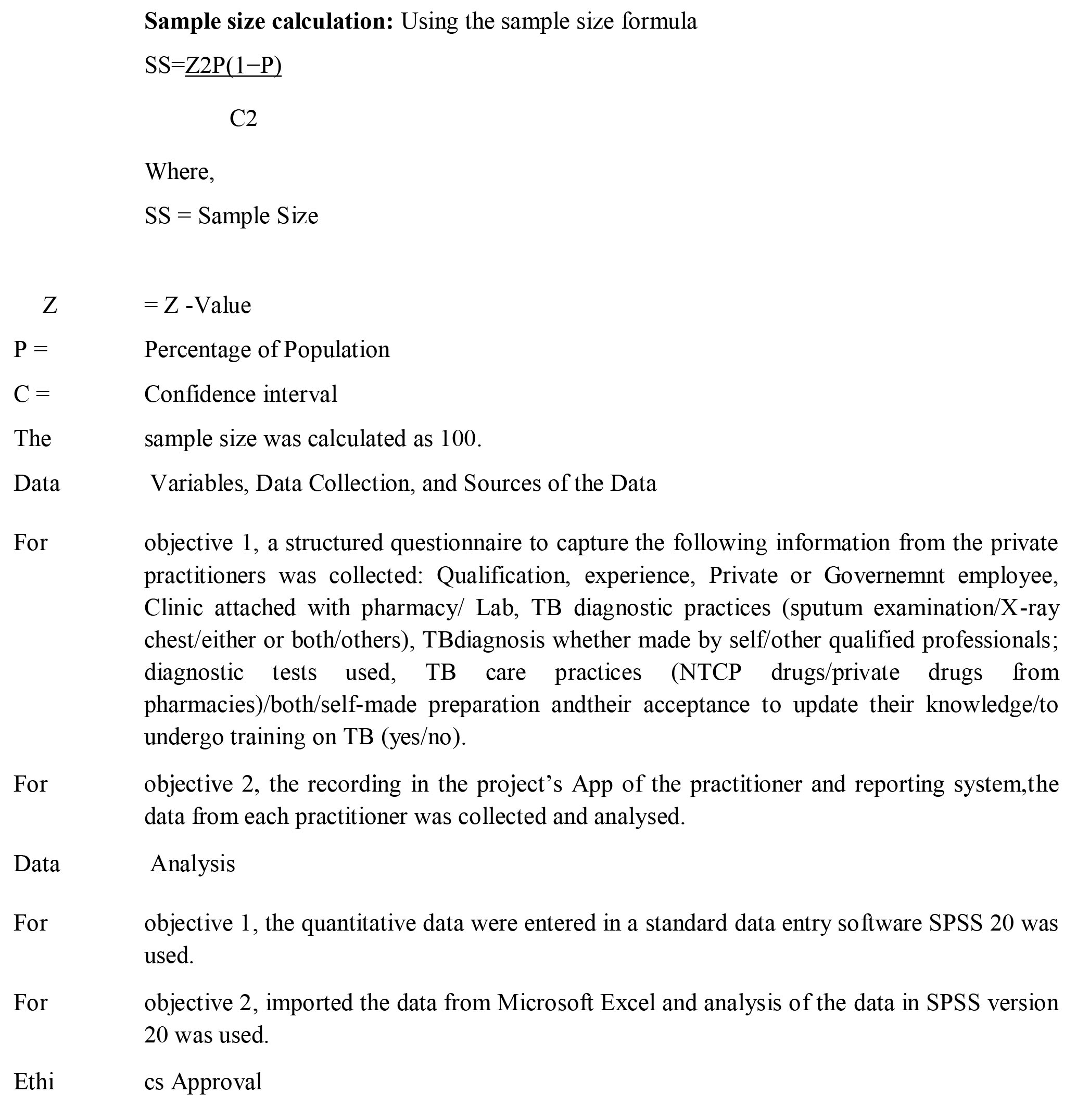
In total out of 100 Practitioners selected initially for this study 94 (94%) practitioners participated. Among the 94 Practitioners 76 (80.85%) were private practitioners, and the remaining 18 Practitioners (19.14%) were practicing in both the private and public sector. A very good Knowledge and attitude towards the standards of TB Care in India (STCI) and National Tuberculosis Control Programme (NTCP) was observed in 90/94 (95.74%) of the participants. 04/94 (04.25%) Practitioners were not aware of the National Programmes. Among the 94 Practitioners88 of them (93.61%) of accepted that STIC and NTCP are necessary and should be implemented vigorously to control TB burden in the country.06/94 (06.38%) of the Practitioners were not in agreement with the implementation of the STCI. (Table 1)TB disease notification to the Government of India Authorities through the proper channel was acceptable among the 79/94 (84.04%) of the Private and Public sector Practitioners. 09/94 (09.57%) of the total 98 Practitioners reported that they were not willing to report. 04/94 (04.25%) participants stated that they are willing to do notification in some cases. 02/92 (02.12%) participants did not answer the section. (Table 1)One major reason given by the Practitioners for not willing to notify the TB case to the Government Authorities was the fear of the social stigma to the family members of the TB case.
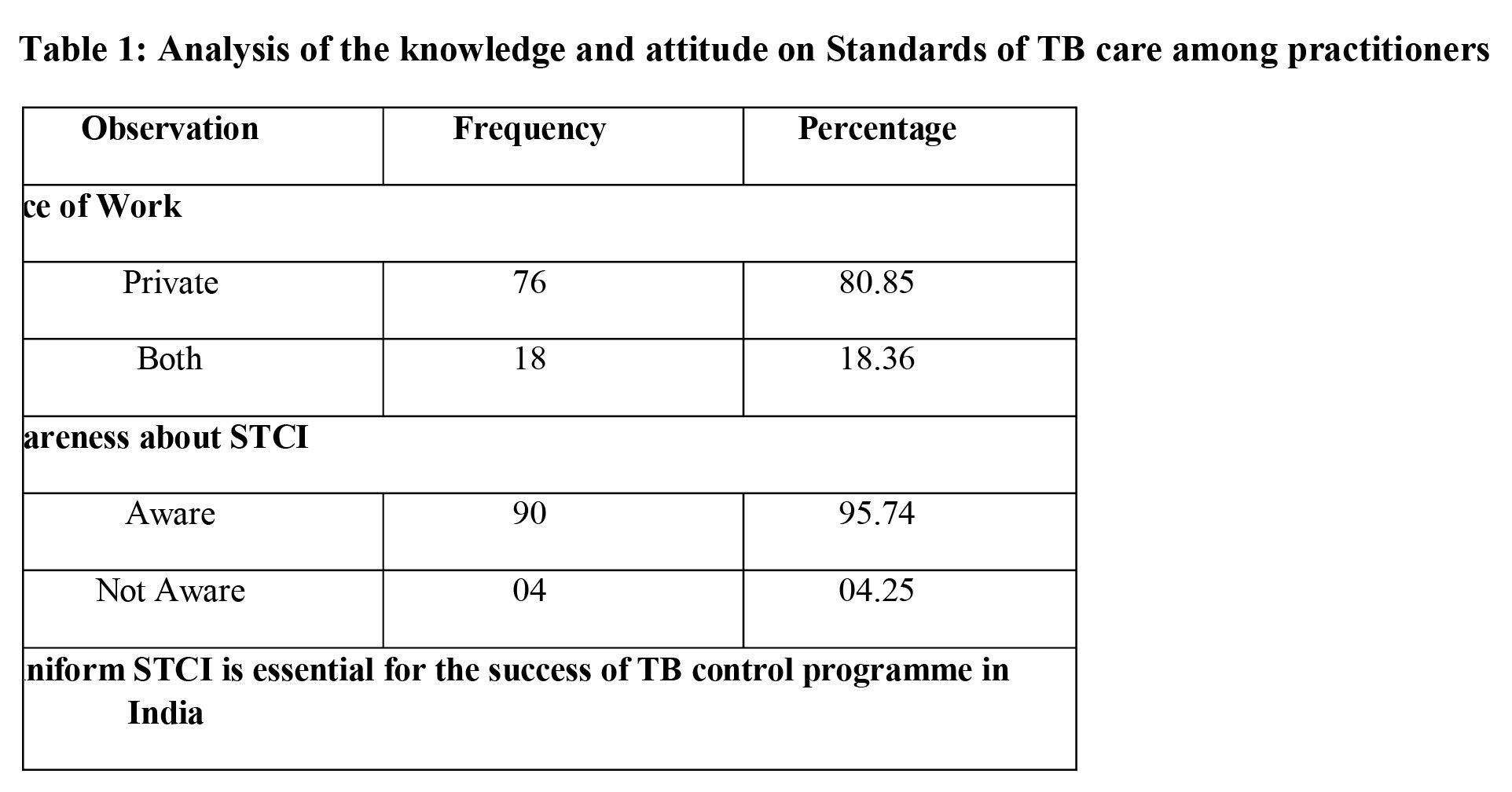
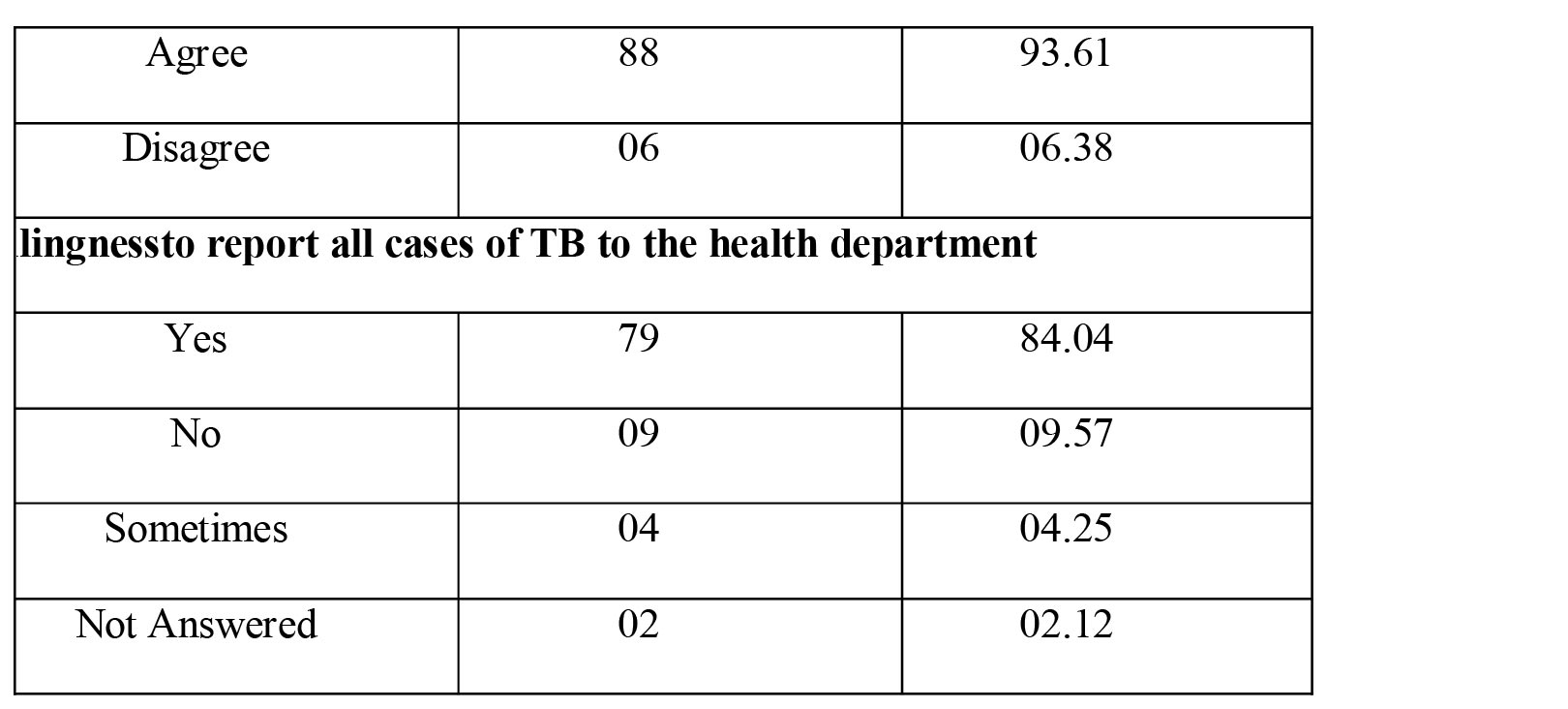
Table 1: Showing the Knowledge and attitude of practitioners towards National Programme for
control of TB (n-94).
Practice:
Prescribing protocols and methods among the Practitioners were observed and found that among the
94participants, 90 (95.74%) were prescribing anti TB drugs for their TB patients. 04
Practitioners (04.25%) reported as not prescribing Anti TB Drugs. Among the 90
Practitioners prescribing anti TB drugs 46/90 (51.11%), were prescribing four drug regimen
with appropriate dosages and duration for TB. 14/90 (15.55%) practitioners were not
following the anti TB regimen and either prescribing 3 drugs , 02 drugs or 01 drug for their
TB patients which was not in agreement with the National Programme. 30/90 (33.33%)
practitioners did not answer the questions related to prescribing practices adopted by them.
(Table 2) The question related to the total duration of anti TB treatment was answered by
68/90 (75.55%) practitioners that anti TB treatment was given for 6 months to the TB
patients. 06/90 (06.66%) practitioners answered as 1 to 05 months. 16/90 (17.77%)
practitioners answered as 07 to 08 months. (Table 2)
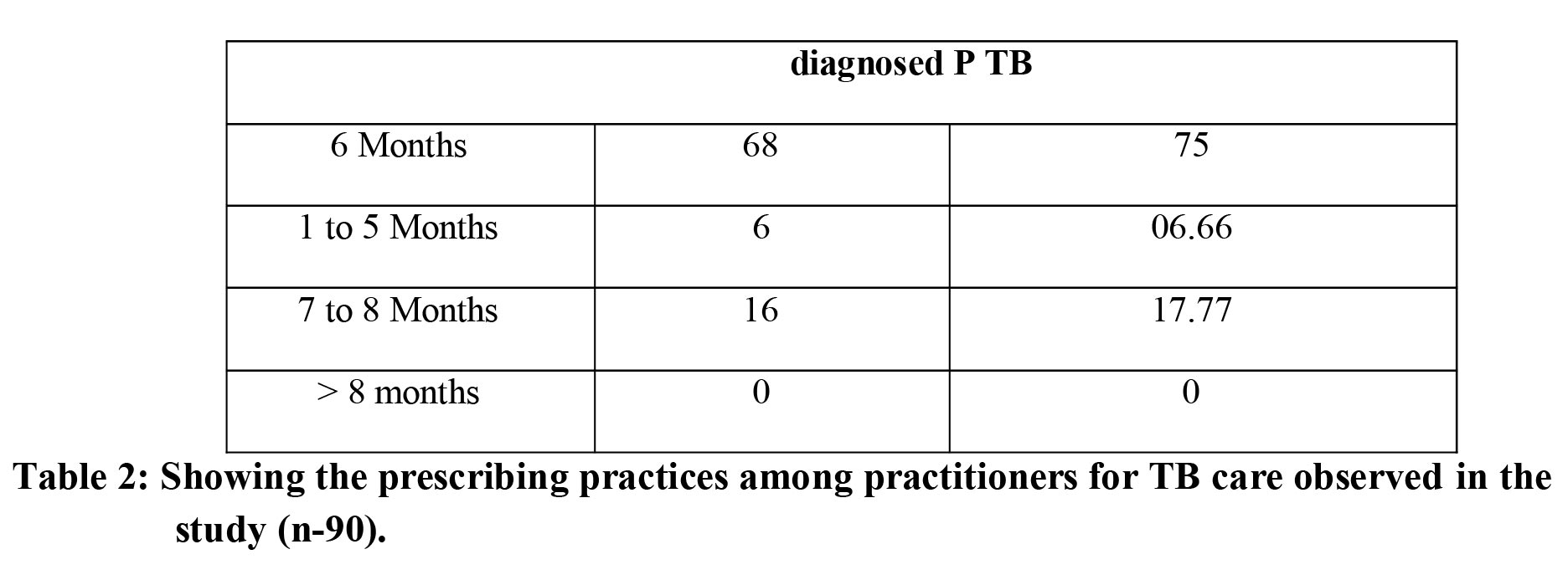 Table 2: Showing the prescribing practices among practitioners for TB care observed in the
study (n-90).
Table 2: Showing the prescribing practices among practitioners for TB care observed in the
study (n-90).
In the self administered questionnaire the participants were asked, aiming to analyse the confidence
with which the practitioners would know the follow up status of the patients till they
complete the anti TB treatment and care. Each one of the practitioners were given a scenario
to recollect and mention the number of TB patients they had prescribed or sent them to
Governemnt Clinics or Hospitals to receive NTEP drugs as well as the number of TB
patients having completed treatment for the prescribed duration; where the denominator of
patients was given as 10 for both scenarios. The observed data was given in Table 3. 44/94
(46.80%) of the practitioners could recall all the 10 TB patients having received the complete
anti TB treatment. 40/94 (42.55%) of the practitioners did not chose to answer the question.
The remaining 10 (10.63%) practitioners answered as between 02 to 09 patients had received
complete treatment. (Table 3). Similarly to the question as to how many patients could have
completed anti TB patients among the last 10 patients treated by them 40/94 (42.55%) did
not chose to answer the question. 34/94 (36.17%) practitioners answered as the last 10
patients had completed the anti TB treatment and care. 08/94 (08.51%) practitioners could
recollect 06 to 08 patients had completed their treatment. 12/94 12.76(%) practitioners could
recollect 07 to 09 patients had completed their anti TB treatment. (Table 3).
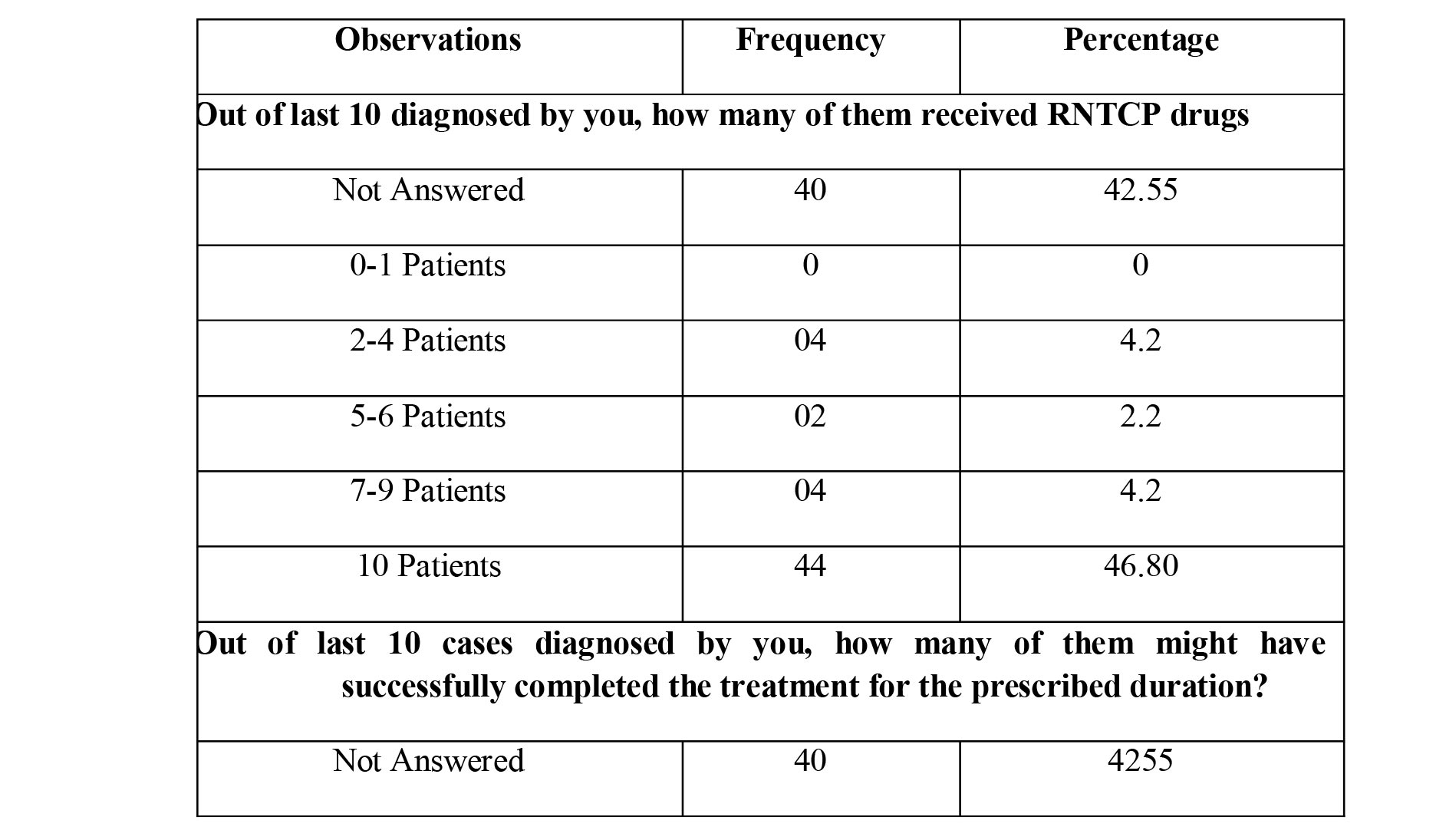
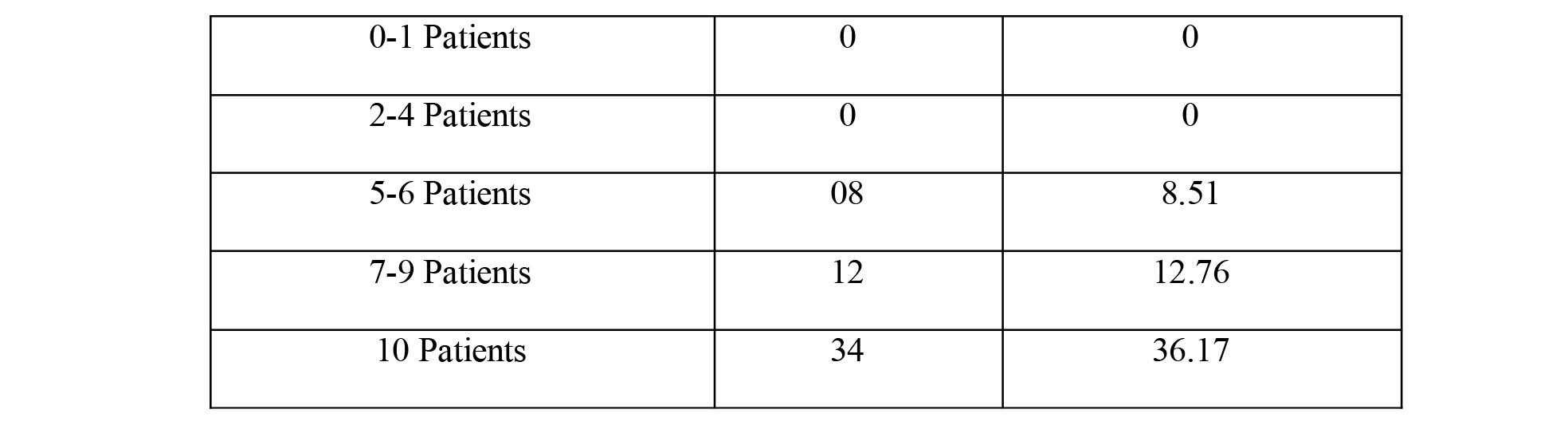
Table 3: Showing the Knowledge of the practitioners regarding treatment and follow up of their patients who received ATT after the diagnosis (n-94).
DISCUSSION:
I n Kerala, under the National Strategic Plan for tuberculosis elimination (NTEP) which is in the phase of TB elimination and aims to eliminate TB by 2025 active work is being undertaken by both private and Governemnt Health agencies. (60) To achieve this target participation of private sector is crucial. Therefore, understanding the Knowledge, Attitude and Practice of private modern medical practitioners was very important for fulfilling this aim. Hence the present study was undertaken to understand the status of private practitioners' involvement in NTEP. Standards for TB Care in India, were developed to implement a uniform strategy of management to all TB patients in India regardless of where they are getting the diagnostic services or receiving the treatment. Thus, the awareness regarding STCI is an important factor when dealing with TB Elimination.This studyshowed that almost all the participants were aware of STCI but still there were gaps in knowledge that needs to be addressed. This can be addressed through more training sessions or interactive sessions and programmes to include both private practitioners and Governemnt Hospital doctors conducted by the State Health Authorities or Indian Medical Association (IMA) or )concerned Non-Governemnt organizationsto reach out all the practitioners. (61) Similar studies conducted and reported from different parts of the country showed variable about knowledge, attitude and practices of TB care among the practitioners. A Study done by Udwadia ZF et al in Mumbai during 2019 (62) showed, only 06 of the 106 respondent practitioners prescribed what could be considered as an appropriate drug regimen recommended by NTEP; with correct drugs, dosage and duration. In their study they observed that 106 practitioners included, prescribed 63 different drug regimens for treatment of TB.A similar study conducted by Rakesh PS et al (63) in Kerala showed 95% of the participants wrote all 4 drugs in intensive phase. This study was conducted in Kerala showed "under treatment for tuberculosis" in private sector was low and more than 80% of doctors were of the opinion that they are sure about follow up and treatment outcome of their not less than 80% patients. Regarding the standards of TB care in India (STCI) observed in the present study showed Awareness about standards of TB Care in India was reported by 95.74% of the participants, and 93.61% of them agreed with the need of STCI to control TB burden in the country.(Table 1)Notification of Tuberculosis to Government of India through proper channel, while treating by any medical practitioner was made mandatory with a gazette notification. (64) TB disease notification to the Government of India Authorities through the proper channel was acceptable among the 79/94 (84.04%) of the Private and Public sector Practitioners. 09/94 (09.57%) of the total 98 Practitioners reported that they were not willing to report. 04/94 (04.25%) participants stated that they are willing to do notification in some cases. 02/92 (02.12%) participants did not answer the section. (Table 1)One major reason given by the Practitioners for not willing to notify the TB case to the Government Authorities was the fear of the social stigma to the family members of the TB case. In regards to the prescription practices and duration of treatment for TB care, this study found that there was an urgent need to spread and popularize the guidelines of TB care to all the medical practitioners in Governemnt and Private sectors, as the country is aiming for total TB elimination from the country. The results also revealed that most of the practitioners are willing to refer their patient to NTEP or treat with NTEP drugs and some are confident regarding treatment completion of their patients which must be expected to be followed by all the practitioners of the state. In the study conducted by Rakesh PS et al (63), they showed that all their 124 participants prescribed anti-TB regimen for 6 months. Whereas in the present study it was observed that only 95.74% were prescribing anti-TB treatment.Similarly, a study done in Mumbai by Udwadia ZF et al (62) showed that only 47% of their 106 participants prescribed the regimen with correct duration. Comparing the drug prescribing practices in the present study, it was observed that 51.1% of the 94 participants had prescribed four drug prescription, which was better than a similar study from Mumbai by Udwadia ZF et al, which reported only 06 of 106 participants prescribed a four drug regimen (62). But the study conducted by Rakesh PS et al (63) showed 94.4% of their participants prescribed all the four drugs in their prescriptions. The Rakesh PS et al study (63) also mentioned that 67 out of 81 (82.71%) private doctors where confident about treatment completion of all their 100% patients in the correct duration. In contrast the present study revealed 36.1% participants were confident regarding completion of anti TB treatment for a NTEP prescribed duration. In the present study the lower response of follow up revealed by the practitioners in these neighbouring districts belonging to two different states, could be due to patients belonging to neighbouring state might have missed the followup at the doctor prescribing the anti TB regimens.
CONCLUSIONS:
The Knowledge, Attitude and Practices of Medical Practitioners working in border districts of Kerala and Karnataka towards Standards of Tuberculosis Care was reasonably good. Even though patients belonged to separate states, notification of cases to Government of India through proper channel was good among the medical practitioners.
Limitation of this study was smaller sample size. Study itself conducted in the border districts of two neighbouring states and one border only.
Recommendations:
Even though sample size was low, this study had a major implication for understanding and improvement of Standards of TB Care in the inter border districts of India. We recommend more such studies in various other districts at interstate borders of India. The strength of this study was that it was the first of its kind involving the medical practitioners of two states of India. We recommend having a meeting of two border district health authorities to discuss the issue of medical practitioners, as they are unaware of the treatment outcome of the border patients who are shifted to other states. This to be conducted in all borders of both the states and to be done in all over India.
Acknowledgement: Authors express their sincere thanks to Dr Badarudheen, DTO, Dakshina Kannada, Dr Amina T P, DTO Kasaragod Dr Shibu Balakrishnan, Regional Consultant (South India), WHO. Dr. Rakesh PS Medical consultant world health organisation, National TB eradication programme -technical assistance project
References:
- Global TB Report 2019: WHO/CDS/TB/2019.23 © World Health Organization 2019; https://www.who.int/tb/publications/global_report/en/
- 3] Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Global Health 2018;6(11):e1196-252.
- World Health Organization, Others. Global tuberculosis report2018. 2018.
- Naidoo P, Theron G, Rangaka MX, et al. The South African tuberculosis care cascade: estimated losses and methodological challenges. J Infect Dis 2017;216:S702-13.
- Subbaraman R, Nathavitharana RR, Satyanarayana S, et al. The tuberculosis cascade of care in India's public sector: a systematic review and meta-analysis. PLoS Med 2016;13:e1002149.
- World Health Organization. Tuberculosis in China. accessed 8 May2019. http:// ww.wpro.who.int/china/mediacentre/factsheets/tuberculosis/en/.
- Commonwealth Fund. International health policy survey. 2013.
- Review on Antimicrobial Resistance. Tackling drug-resistant infections globally: final report and recommendations. May, 2016. Available athttps://amr-review.org/ sites/default/files/160518_Final%20paper_with%20cover.pdf. Accessed April 20, 2019.
- World Health Organization. Global tuberculosis report2018. Geneva, Switzerland. 2018. ISBN 978-92-4-156564-6.
- Kruk M, Gage A, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Global Health 2018:e1196-252.
- Shah NS, Auld S, Brust J, et al. Transmission of extensively drug-resistant tuberculosis in South Africa. N Engl J Med 2017;376:243-53.
- Keshavjee S, Farmer PE. Tuberculosis, drug resistance, and the history of modern medicine. N Engl J Med 2012;367(September (10)):931-6.
- Laxmeshwar C, Stewart A, Dalal A, et al. Beyond "cure" and "treatment success": quality of life of patients with multidrug-resistant tuberculosis. Int J Tuberc Lung Dis 2019;23(1):73-81.
- Byabagambi J, Marks P, Megere H, Karamagi E, Byakika S, Opio A, et al. Improving the quality of voluntary medical male circumcision through use of the continuous quality improvement Approach: A pilot in 30 PEPFAR-Supported sites in uganda. PLoS ONE 2015;10:e0133369https://doi.org/10.1371/journal.pone.0133369.
- Ikeda DJ, Nyblade L, Srithanaviboonchai K, Agins BD. A quality improvement approach to the reduction of HIV-related stigma and discrimination in healthcare settings. BMJ Global Health 2019;4:e001587https://doi.org/10.1136/bmjgh-2019- 001587.
- Sato A., Ramesh K.Why care about quality of care?The case of Lao PDR n.d.
- Global tuberculosis report 2018. Geneva: World Health Organization; 2018.
- Stop TB Partnership. United Nations high level meeting on tuberculosis: key targets and commitments. http://www.stoptb.org/global/advocacy/unhlm_targets.asp; 2018 [accessed 29/04/2019].
- Guo N, Marra CA, Marra F, Moadebi S, Elwood RK, Fitzgerald JM. Health state utilities in latent and active tuberculosis. Value Health 2008;11(7):1154-61. https://doi.org/10.1111/j.1524-4733.2008.00355.x.
- Chamla D. The assessment of patients' health-related quality of life during tuberculosis treatment in Wuhan, China. Int J Tuberc Lung Dis 2004;8(9):1100-6.
- Rajeswari R, Muniyandi M, Balasubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental and social well-being: a field report from south India. Soc Sci Med 2005;60(8):1845-53. https://doi.org/10. 1016/j.socscimed.2004.08.024.
- Padayatchi N, Daftary A, Naidu N, Naidoo K, Pai M. Tuberculosis: treatment failure, or failure to treat? Lessons from India and South Africa. BMJ Glob Health 2019;4(1):e001097.
- WHO. Global tuberculosis report in Geneva. World Health Organization; 2018. CC BY-NC-SA 3.0 IGO.
- World Health Organization. The end TB strategy. Global strategy and targets for tuberculosis prevention, care and control after 2015. Geneva: WHO; 2014. p. 2.
- UNAIDS. Tuberculosis and HIV UNAIDS. Joint United Nations Programme on HIV/ AIDS; 2019.
- World Health Organization. The end TB strategy. In: World Health Organization2014.
- World Health Organization. The global plan to stop TB 2011-2015: transforming the fight towards elimination of tuberculosis. 2010, World Health Organization.
- Karumbi J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database Syst Rev 2015(5). https://doi.org/10.1002/14651858.CD003343.pub4. Cd003343PMID: 26022367.
- Sreeramareddy CT, Qin ZZ, Satyanarayana S, Subbaraman R, Pai M. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis 2014;18(3):255-66.
- Subbaraman R, Nathavitharana RR, Satyanarayana S, Pai M, Thomas BE, Chadha VK, et al. The tuberculosis cascade of care in india's public sector: a systematic review and meta-analysis. PLoS Med 2016;13(10):e1002149https://doi.org/10. 1371/journal.pmed.1002149. PMID: 27780217.
- Naidoo P, Theron G, Rangaka MX, Chihota VN, Vaughan L, Brey ZO, et al. The south african tuberculosis care cascade: estimated losses and methodological challenges. J Infect Dis 2017;216(suppl_7):S702-13. https://doi.org/10.1093/ infdis/jix335. PMID: 29117342.
- Subbaraman R, Nathavitharana RR, Mayer KH, Satyanarayana S, Chadha VK, Arinaminpathy N, et al. Constructing care cascades for active tuberculosis: a strategy for program monitoring and identifying gaps in quality of care. PLoS Med 2019;16(2):e1002754https://doi.org/10.1371/journal.pmed.1002754. PMID: 30811385.
- WHO. Global TB Report. 2019 October 17 2019. Report No.
- Dodd PJ, Yuen CM, Sismanidis C, Seddon JA, Jenkins HE. The global burden of tuberculosis mortality in children: a mathematical modelling study. The Lancet Global Health 2017;5(9):e898-906.
- WHO. Global TB Report. 2019 October 17 2019. Report No.
- Dodd PJ, Yuen CM, Sismanidis C, Seddon JA, Jenkins HE. The global burden of tuberculosis mortality in children: a mathematical modelling study. The Lancet Global Health 2017;5(9):e898-906.
- WHO. TB country profile-South Africa. 2018.
- World Health Organization. Engaging private health care providers in TB care and prevention: a landscape analysis. Geneva: World Health Organization; 2018.
- World Health Organization. The stop TB strategy: building on and enhancing dots to meet the TB-related millennium development goals. Geneva: World Health Organization; 2006.
- World Health Organization. Engaging all health care providers in TB control: guidance on implementing public-private mix approaches. Geneva: World Health Organization; 2006.
- World Health Organization. Engaging all health care providers in TB control: guidance on implementing public-private mix approaches. Geneva: World Health Organization; 2006.
- World Health Organization. Global tuberculosis report 2018. 2018.
- Houben RM, Dodd PJ. The global burden of latent tuberculosis infection: a re-estimation using mathematical modelling. PLoS Med 2016;13(10):e1002152.
- World Health Organization. A patient centered approach to care 2018 [Available from: https://apps.who.int/iris/bitstream/handle/10665/272467/WHO-CDS-TB2018.13-eng.pdf.
- Das J, Kwan A, Daniels B, Satyanarayana S, Subbaraman R, Bergkvist S, et al. Use of standardized patients to assess quality of tuberculosis care: a pilot, cross-sectional study. Lancet Infect Dis 2015;15(11):1305-13.
- The end TB strategy: Global strategy and targets for tuberculosis prevention, care and control after 2015. Geneva: World Health Organization; 2014 Available at http://www.who.int/tb/strategy/End_TB_Strategy.pdf Accessed on June 2019.
- Toman K. Tuberculosis case-finding and chemotherapy: Questions and answers. GenevaSwitzerland: World Health Organization; 1979. 1211 27.
- Reid MJA, Arinaminpathy N, Bloom A, et al. Building a tuberculosis-free world: the Lancet Commission on tuberculosis. Lancet 2019;393(10178):1331-84.
- Cazabon D, Alsdurf H, Satyanarayana S, et al. Quality of tuberculosis care in high burden countries: the urgent need to address gaps in the care cascade. Int J Infect Dis 2017;56:111-6.
- World Health Organization. Quality of care: a process for making strategic choices in health systems. Geneva: WHO; 2006. [Google Scholar].
- Mackintosh M, et al. Universal health coverage: markets, profit and the public good (series). Lancet 2016;388.
- WHO, "Global tuberculosis report," World Health Organization, Geneva, 2019.
- Pai M, Temesgen Z. Quality: the missing ingredient in TB care and control. J Clin Tuberc Other Mycobact Dis 2019;14:12-3.
- Daniels B, Kwan A, Pai M, Das J. Lessons on the quality of tuberculosis diagnosis from standardized patients in China, India, Kenya, and South Africa. J Clin Tuberc Other Mycobact Dis 2019;16:100109.
- Udwadia Z, Furin J. Quality of drug-resistant tuberculosis care: Gaps and solutions. J Clin Tuberc Other Mycobact Dis 2019;16:100101.
- Arinaminpathy N, Batra D, Khaparde S, Vualnam T, Maheshwari N,Sharma L, Nair SA, Dewan P. The number of privately treatedtuberculosis cases in India: estimation from drug sales data. Lancet Infect Dis 2016;16:1255-1260.
- Mackintosh M, Channon A, Karan A, Selvaraj S, Cavagnero E, Zhao H. What is the private sector? Understanding private provision in the health systems of low-income and middle-income countries. Lancet. 2016;388(10044):596‐605. doi:10.1016/S0140-6736(16)00342-1.
- Arsenault C, Roder-DeWan S, Kruk ME. Measuring and improving the quality of tuberculosis care: a framework and implications from the Lancet Global Health Commission. J Clin Tuberc Other Mycobact Dis 2019;16:100112.
- Ikeda DJ, Basenero A, Murungu J, Jasmin M, Inimah M, Agins BD. Implementing quality improvement in tuberculosis programming: lessons learned from the global HIV response. J Clin Tuberc Other Mycobact Dis 2019;17:100116.
- National Strategic Plan for Tuberculosis Eliminnation 2017-2025. Revised nationaltuberculosis control program. Central TB Division, Directorate General of HealthServices, Ministry of Health with FamilyWelfare.2017.https://tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf
- National Strategic Plan for Tuberculosis Eliminnation 2017-2025. Revised nationaltuberculosis control program. Central TB Division, Directorate General of HealthServices, Ministry of Health with FamilyWelfare.2017.https://tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf
- Udwadia ZF, Pinto LM, Uplekar MW. Tuberculosis management by private practitioners in Mumbai, India: has anything changed in two decades? PLoS One 2010;5(8):e12023.
- Rakesh PS, Balakrishnan S, Jayasankar S, Asokan RV. TB management by private practitioners - Is it bad everywhere? The Indian Journal of Tuberculosis. 2016;63(4):251-254.
- The Gazette of India REGD. NO. D. L.-33004/99 NEW DELHI, MONDAY, MARCH 19, 2018/PHALGUNA 28, 1939 :Department of Health and Family Welfare http://egazette.nic.in/WriteReadData/2018/183924.pdf
