Subscribe now to get notified about IU Jharkhand journal updates!
The Role of Digital Technologies in Enhancing Access to Healthcare for Marginalized
Abstract :
The Covid crisis has the taught the whole world the importance of proper healthcare facilities and the role which new age digital technologies can play in improving it. When the crisis began, we witnessed systemic failure of health care infrastructure. The worst hit were the people from marginalized communities and areas without any proper healthcare infrastructure and facilities. But within a short span of time, digital transformation helped these people through telemedicine, remote monitoring, contact tracing, etc. This proved that although upgrading the health infrastructure can take some time, through use to digital technology, the best use to existing facilities can be done in much more efficient manner.
However, greater reliance on digital tools has the potential to increase disparities between those who have skills and access to digital tools and those who do not and thereby existing health disparities. It is therefore important that these new age technologies are not only used to provide health facilities, but are used in such manner that the ones with minimum resources are also covered by its benefits. This paper, will explore the role that digital technologies can play Enhancing access to Healthcare for Marginalized People. The paper will also highlight the existing problems which are hindrance in digital transformation in health care sector.
Keywords :
Health Care, Digital Transformation, Technology, Telemedicine, Marginalized People.Introduction
Digital and technological innovations are having a significant impact on everyday life, transforming the way people work, communicate, and access information. These innovations have brought about a wide range of benefits, such as improved efficiency, convenience, and accessibility. They have also created new opportunities for collaboration, learning, and innovation. It has enabled businesses to streamline their operations, automate routine tasks, and reduce costs. This has led to increased productivity and improved efficiency in many industries. It has made it easier for people to access information, products, and services from the comfort of their own homes. This has made life more convenient and has saved people time and effort. It has made it easier for people to collaborate and work together, regardless of their location and transformed the way people learn, enabling online education, virtual classrooms, and educational apps.
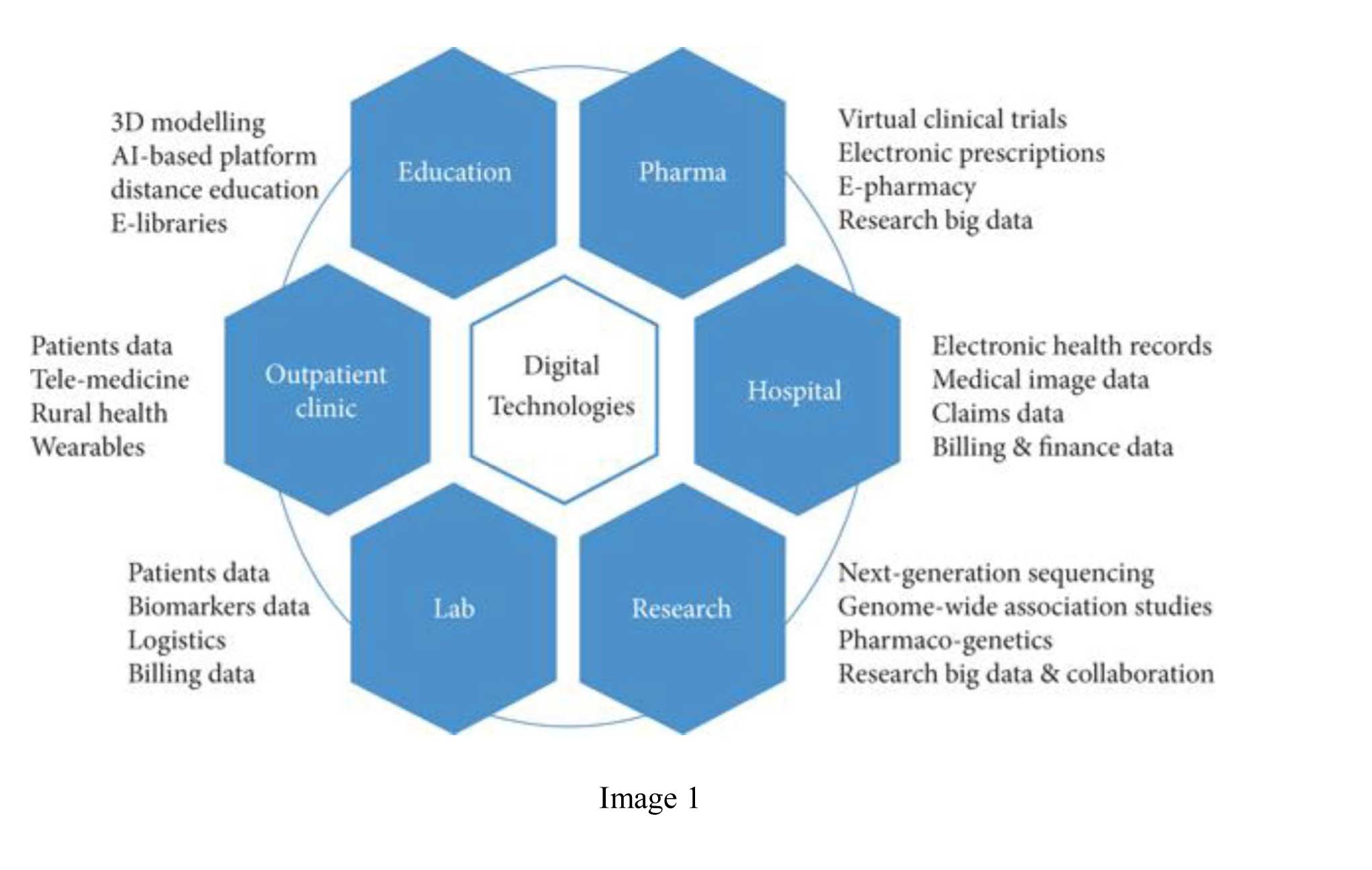
The one area where the digital technologies have the potential to revolutionize the existing system is healthcare delivery and access to healthcare services, particularly for marginalized populations(Sascha et al., 2021). Marginalized populations often face significant barriers to accessing traditional healthcare services, such as geographic isolation, lack of transportation, and many other socioeconomic factors. Digital technologies such as telemedicine, mobile health (mHealth) apps, remote patient monitoring, AI tools, smart devices and health information systems can help bridge the gap and provide healthcare services to those who need it the most(Sayani et al., 2019). By leveraging these technologies, healthcare providers can reach patients in remote or underserved areas, monitor patients' health remotely, and improve coordination of care across multiple providers.
One of the most interesting development in this field is the use of artificial intelligence (AI) in biomedicine, healthcare, and medical education(Wainstein, 2018). AI has the potential to greatly enhance the functionality and performance of diagnostic tools. Also, it might help with treatment process improvement, resulting in higher therapeutic effectiveness, happier patients, and cheaper costs(J X He et al., 2019). It is therefore important to ensure that digital technologies are accessible, affordable, and integrated into existing healthcare systems in a way that complements and enhances traditional healthcare services.
With the introduction of the 2030 Agenda for Sustainable Development, the world has made a commitment to leaving no one behind by putting an end to extreme poverty and preventable child deaths and by encouraging sector-wide coordinated action to address challenging development issues. UNICEF has recently launched both its new Strategic Plan, 2018–2021(UNICEF, 2018) and the Strategy for Health, 2016–2030(UNICEF, 2015). The Strategy for Health has two overarching goals:
1) end preventable, maternal, newborn and child deaths; and
2) promote the health and development of all children.
To achieve these targets, several new and innovative approaches needs to be taken and use of digital technology is one of the most important among them.
More than 7 billion people (95 per cent of the global population) live in an area that is covered by a mobile-cellular network, and nearly 41 per cent of people in developing countries have a mobile broadband subscription(ITU, 2016) . Advances in technology, such as improved network speed and efficiency, cloud computing, device connectivity and data analytics are accelerating conversations on the promise of digital health. In this context, countries with limited resources like India can harness the power of information and communication technologies (ICT) to effectively ensure that everyone gets access to health services.
While the anecdotal trends suggest the expansion of digital technologies normally happens in metropolitan centres, India's data reveal a different tale. According to ICEA, mobile phones primarily contributed to a 35% annual increase in internet users in rural India and a 7% increase in urban areas in 2018. Smartphone penetration in rural India increased from 9% in 2015 to 25% in 2018. This shows the potential up to which digital transformation can facilitate the health care accessibility in India.
Digital Health - A New Way Forward
The traditional healthcare system is centred mostly on the delivery of medical services through networks of hospitals and outpatient clinics. The qualifications of medical staff, hospital infrastructure, and the availability of modern equipment are only a few of the numerous variables that affect how well a health service is provided. But due to the rapid advancement of technology and the public's demand for high-quality medical care, such a traditional platform has recently been confronted with new difficulties. This problem can be solved by implementing Digital Health initiatives.
The term ‘digital health’, which includes both mHealth and eHealth, was just recently coined as "a broad umbrella word including eHealth (which includes mHealth) as well as developing disciplines, such as the application of sophisticated computing sciences in big data, genomics, and artificial intelligence(WHO, 2016). eHealth can be defined as the use of information and communications technology in support of health and health-related sectors. The use of mobile wireless technology for health is referred to as mobile health (mHealth), which is a subset of eHealth.
While digital health initiatives can only support the traditional health care system, it has potential to make sure that complete use of existing system can be done. At a much lower investment, the reach of traditional health care infrastructure can be enhanced up to optimal levels.
II. Policy Areas in Focus
While there are several areas in healthcare where use of technology can further enhance accessibility and affordability, some of the major ones are telemedicine, remote monitoring, contact tracing, health information systems, smart devices and use of AI in health care. These areas are disscused below-
1. Telemedicine - Telemedicine allows healthcare providers to deliver care to patients remotely, using videoconferencing and other digital communication technologies. This can be particularly beneficial for marginalized populations living in rural or remote areas, who may not have access to traditional healthcare services. It has gained significant traction in India, particularly in recent years. With a large and diverse population, many of whom live in remote or underserved areas, India has significant healthcare challenges, and telemedicine offers a potential solution to improve healthcare access and delivery.
In 2018, the Indian government launched the National Telemedicine Service under the name eSvanjivaniOPD, which aims to provide telemedicine services to all primary health centers in the country. The service uses a hub-and-spoke model, with specialist doctors located in hub centers providing teleconsultation services to patients at spoke centers(S Mishra et al., 2019). This has helped improve access to specialized care for patients living in remote or underserved areas.
Private companies have also played a significant role in the growth of telemedicine in India, with several telemedicine startups emerging in recent years. These startups use mobile apps and other digital platforms to connect patients with healthcare providers, allowing patients to access care from the comfort of their own homes. Some of the major Indian private sector players in telemedicine include Narayana Hrudayalaya, Apollo Telemedicine Enterprises, Asia Heart Foundation, Escorts Heart Institute, Amrita Institute of Medical Sciences, and Aravind Eye Care(Das & Deb, 2008).
However, despite the growth of telemedicine in India, there are still significant challenges to overcome. These include the need for better infrastructure and connectivity in remote areas, as well as regulatory challenges related to telemedicine practice and reimbursement. Additionally, there is a need to ensure that telemedicine services are accessible and affordable to all, particularly marginalized populations who may face additional barriers to accessing healthcare services.
Therefore, telemedicine has the potential to improve healthcare delivery and access in India, particularly for marginalized populations living in remote or underserved areas. However, ongoing investment and innovation will be needed to ensure that telemedicine services are effective, accessible, and equitable for all(Ashley, 2002).
2. Mobile health (mHealth) apps: mHealth apps allow patients to monitor their health, track their medications, and communicate with healthcare providers using their smartphones or other mobile devices. This can be particularly beneficial for marginalized populations who may have limited access to healthcare facilities or who may face transportation barriers. With the decreasing prices of smartphones and internet, people from marginalized population can easily avail these benefits.
Mobile health (mHealth) apps are gaining popularity in India, particularly as smartphone use continues to grow across the country. mHealth apps offer a range of benefits, including improved access to healthcare information and services, increased patient engagement, and better health outcomes.
There are several mHealth apps that are currently popular in India, including:
a. Practo: Practo is a popular mHealth app in India that allows users to search for and book appointments with doctors, as well as order medicines and book lab tests.
b. Netmeds: Netmeds is an online pharmacy that allows users to order medicines and other healthcare products online and have them delivered to their homes.
c. 1mg: 1mg is an mHealth app that provides users with access to healthcare information, including drug information, and allows users to book lab tests and order medicines online.
d. MyFitnessPal: MyFitnessPal is a popular health and fitness app that allows users to track their diet, exercise, and other health metrics.
e. mfine: mfine is an mHealth app that provides users with access to online consultations with doctors and specialists, as well as online diagnostic tests and medicine delivery.
These apps are particularly beneficial for people living in remote or underserved areas, who may have limited access to healthcare services. They can also be useful for people with chronic conditions, who may need to monitor their health regularly and access healthcare services more frequently.
The major challenges to the growth of mHealth apps in India, including the need for better infrastructure and connectivity in remote areas, as well as the need to ensure that these apps are accessible, affordable and developed in user friendly manner. The language barrier can be another concern in large and diverse country like India. Additionally, there are serious concerns around the quality and reliability of healthcare information provided through these apps, and the need to ensure that user data is protected and secure. Another issue concerning the same is the cost of these services. Without regulating cost and providing incentives, the reach of these mHealth apps may be limited to only urban areas.
3. Remote patient monitoring: Remote patient monitoring(RPM) allows healthcare providers to monitor patients' health remotely, using digital technologies such as wearable devices and sensors without the need for in-person visits.. This can be particularly beneficial for marginalized populations with chronic conditions who may require frequent monitoring and support such as Tuberculosis(L. Hogaboam et al., 2018 ). Another major use of RPM can be maintaining track of old patients who need frequent monitoring and its difficult for them to travel (N. van den Berg et al. 2012).
In India, RPM is still in its early stages, but there are a few initiatives underway. For example, in 2019, the Indian government launched the National Digital Health Blueprint, which includes a focus on RPM (Sudip et al, 2022). The blueprint aims to create a national digital health ecosystem that will enable RPM, as well as other digital health services, to be scaled up across the country.
Private companies are also beginning to explore RPM in India. For example, in 2020, Medtronic launched its Guardian Connect continuous glucose monitoring system in India. The system allows people with diabetes to monitor their blood glucose levels in real-time, and can alert healthcare providers if levels become too high or too low.
4. Health information systems: Health information systems(HIS) allow healthcare providers to access and share patient information securely and efficiently, improving coordination of care and reducing errors. This can be particularly beneficial for marginalized populations who may see multiple providers or who may receive care from different healthcare facilities. Often it is seen that patients from marginalized communities, with low level of education, are unable to clearly inform the doctor about the previous treatments and diagnosis. A robust and comprehensive HIS can solve this problem and medical practitioners may be able to better treat their patient if they already know about previous medical records. It can also help in tracking the patients and monitoring their treatment as many times patients leave the treament in between and this results further deterioration in their health . In Mozambique, a robust electronic patient management system facilitated a facility-level reporting of required indicators, improved ability to identify patients lost to follow-up and support facility and patient management for HIV care(Hochgesang et al., 2017). Similarly in India, DOTS or Directly Observed Therapy Shortcourse for Tubercolosis treatment has applied HIS to follow patient development (Mandal et al., 2017).
Health Information Systems in India refer to the collection, processing, storage, and management of health-related information. HIS play a crucial role in the delivery of healthcare services, providing accurate and timely information to healthcare providers, policymakers, and patients.
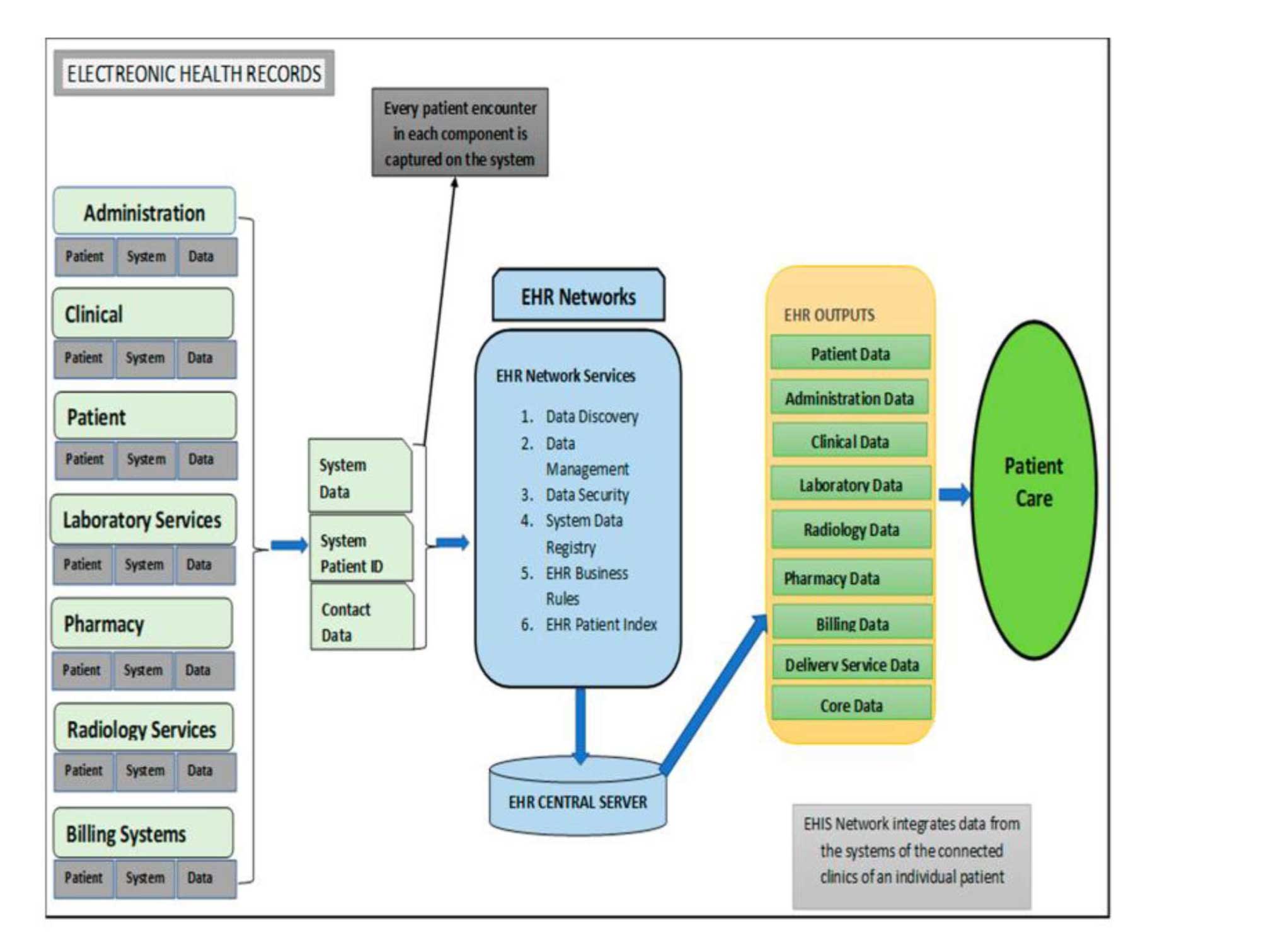
India has made significant progress in implementing HIS over the past decade. The National Health Stack, launched in 2018, is a digital health infrastructure that aims to provide a common platform for healthcare data exchange across the country. The stack comprises a range of digital health solutions, including Electronic Health Records (EHR), telemedicine, and e-pharmacy.
The Indian government has also launched several initiatives to promote the use of HIS at the state and national levels. For example, the Ministry of Health and Family Welfare launched the Integrated Disease Surveillance Programme (IDSP) in 2004, which provides real-time disease surveillance and response to outbreaks.
Other notable HIS initiatives in India include National Health Stack which is a digital health infrastructure that aims to provide a common platform for healthcare data exchange across the country.
Despite these initiatives, challenges remain in the implementation of HIS in India. For example, there is a need to ensure the standardization of data collection and management across different healthcare facilities and systems. Additionally, there is a need for greater investment in HIS infrastructure and training for healthcare providers to ensure that HIS are effectively utilized. Another major problem concerning it is the privacy of the data stored in system. This problem can be well tackled by use of blockchain technology, which has proved itself to be a reliable information storage system.
The HIS has the potential to improve healthcare delivery and access in India, providing timely and accurate information to healthcare providers, policymakers, and patients. However, ongoing investment and innovation will be needed to ensure that HIS are effective, accessible, and equitable for all.
5. Artificial intelligence (AI): If 20th century belonged to computers and internet, the 21st will be dominated by artificial intelligence. AI can be used to analyze large amounts of data and identify patterns and trends that may not be apparent to human healthcare providers. This can help improve diagnosis and treatment, particularly for marginalized populations who may have limited access to specialized healthcare services.
Artificial intelligence (AI) has the potential to revolutionize healthcare delivery, improving patient outcomes and reducing healthcare costs(Hossain et al., 2019). the two major areas in which use of AI and Machine learning can change the whole system are (1) clinical decision making along patient care management and (2) proactive diagnosis (Mistry, 2019). In India, AI has been increasingly adopted in healthcare in recent years, with several initiatives underway.
One key area of AI application in healthcare is radiology and medical imaging analysis. AI algorithms can be trained to analyze medical images, such as Ultrasound, X-rays, MRIs, and CT scans, to help identify and diagnose diseases. Several Indian startups, such as ParallelDots, Niram.ai and Qure.ai, are developing AI-based medical imaging solutions for cancer detection, fracture detection, and more. In developing countries like India, where doctor-population ratio still needs improvement, availability of doctors 24*7 is very difficult. While inexperienced and under-training doctors can still be available, the gap increases multi-fold when it comes to specialized and experienced doctors. It can be seen that 60-70% of work in Indian Medical Colleges are being done by resident under training doctors. It may take years of hard work and patience for these doctors to learn and understand difficult images such as CT scan and MRI, while a AI based machince can master it within minutes if big data is provided accurately. In such a scenario, these technologies can be very useful to immediately identify the serious cases and help medical professionals to optimise their resources.
Another area where AI is being applied in healthcare in India is personalized medicine. AI algorithms can be used to analyze patient data, such as genomics, medical history, and lifestyle factors, to help healthcare providers develop personalized treatment plans. For example, the Indian startup MedGenome is using AI to analyze genetic data to develop personalized cancer treatments.
In addition to medical imaging and personalized medicine, AI is also being used in healthcare in India for disease diagnosis and prediction, drug discovery, and patient monitoring. For example, the Indian company Biofourmis is using AI to monitor patients with heart failure, helping healthcare providers to identify and treat symptoms before they become severe. One of the major cause of deaths because of heart attacks and failure is wrong, delayed or no diagnostics of heart disease. With the use of AI, these problems can be minimized and proper proactive steps can be taken. Many studies have been conducted on the application of AI and machine learning in cardiology. For instance, Attia et al.(2019) investigated whether AI might be used to diagnose asymptomatic left ventricular dysfunction (ALVD) using an electrocardiogram (ECG), a common technique for gauging the electrical activity of the heart. The authors came to the conclusion that the ECG could be used as a powerful screening tool for ALVD in asymptomatic people by using AI to this widely used, affordable test.
However, there are challenges to the widespread adoption of AI in healthcare in India. The lack of standardized data collection and management across different healthcare systems remains of the major issue in this field also. Another problem is resistance of the doctors and other medical professionals to effectively adapt and trust these new age technologies. The need for regulatory frameworks to ensure that AI-based healthcare solutions are safe, effective, and ethical is also must.
Therefore, AI has the potential to significantly improve healthcare delivery and access in India, particularly for marginalized populations who may face significant barriers to accessing traditional healthcare services. Ongoing investment and innovation will be needed to ensure that AI-based healthcare solutions are accessible and equitable for all.
6. Big Data and eHealth - Big data refers to large sets of data that are too complex and massive to be processed by traditional data processing methods. In healthcare, big data refers to large and complex datasets generated by various sources such as electronic health records (EHRs), medical devices, and healthcare claims data. E-health, on the other hand, refers to the use of electronic technologies such as digital health records, mobile health apps, and telemedicine to improve healthcare delivery and outcomes.
The use of big data in e-health can revolutionize healthcare by enabling more personalized and targeted care, improving patient outcomes, and enhancing efficiency in healthcare delivery (Palanisamy & Thirunavukarasu, 2019). By analyzing large and diverse sets of health data, healthcare providers can gain insights into disease patterns, treatment effectiveness, and patient outcomes, allowing them to tailor treatments and interventions to individual patients.
Big data can also be used to develop predictive models for disease outbreaks, enabling public health officials to better manage and respond to epidemics and pandemics(Shafqat et al., 2020). In addition, big data can be used to identify areas where healthcare resources are lacking, helping to improve healthcare access and equity.
7. Smart Devices - Smart devices refer to electronic devices that are connected to the internet or other networks and have the ability to communicate, interact, and exchange data with other devices or systems. These devices are typically equipped with sensors, software, and connectivity features that enable them to collect and transmit data, receive and process information, and perform automated actions.
In healthcare, smart devices have the potential to revolutionize healthcare delivery by enabling remote monitoring, personalized care, and improved patient outcomes. For example, wearable devices such as fitness trackers and smartwatches can collect data on physical activity, heart rate, and other vital signs, which can be used by healthcare providers to develop personalized treatment plans and monitor patient progress.
Smart medical devices such as insulin pumps and blood glucose monitors can also help patients manage chronic conditions more effectively, reducing the need for frequent hospital visits and improving overall quality of life. In addition, smart devices can be used to enable remote consultations and telemedicine, allowing patients to access healthcare services from the comfort of their own homes.
8. Blockchain Technology in Healthcare - Blockchain technology is a decentralized and secure system for recording transactions and data in a transparent and tamper-proof manner. In healthcare, blockchain technology can be used to improve data security, privacy, and interoperability between different healthcare stakeholders.
One of the key benefits of blockchain technology in healthcare is improved data security (Daley, 2020). By storing data on a decentralized ledger that is secured with cryptographic algorithms, blockchain technology makes it more difficult for hackers to gain access to patient data. This is particularly important in healthcare, where sensitive patient data must be protected from unauthorized access and data breaches. Recently we have seen that data of AIIMS Delhi was hacked and leaked by international hackers.
Blockchain technology can also improve data privacy by allowing patients to control how their data is shared and accessed. Patients can use blockchain-based systems to give explicit consent for healthcare providers to access their data, ensuring that their data is only used for authorized purposes and that their privacy is protected.
Another potential benefit of blockchain technology in healthcare is improved interoperability between different healthcare stakeholders. By using a common blockchain-based system, healthcare providers can securely share data with each other in a standardized format, making it easier to exchange information and coordinate care.
There are also potential use cases for blockchain technology in clinical trials, supply chain management, and public health. For example, blockchain technology can be used to track and authenticate the origin of pharmaceutical products, ensuring that they are not counterfeit or tampered with(Hasselgrer et al., 2020).
Despite the potential benefits of blockchain technology in healthcare, there are also significant challenges to overcome, such as regulatory compliance, scalability, and interoperability with existing systems. Nevertheless, many experts believe that blockchain technology has the potential to transform the healthcare industry by improving data security, privacy, and interoperability.
III. Ethical Considerations
The use of digital health technologies, such as HIS, RPM, AI and machine learning, presents ethical considerations that must be addressed to ensure patient privacy, data security, and equity. The primary ethical concerns related to digital health is the protection of patient privacy and misuse of data(Brall et al., 2019). Digital health technologies often collect and store large amounts of personal health data, including sensitive information such as medical histories and genetic data. It is important to ensure that this data is kept secure and confidential, and that patients have control over how their data is used and shared. Blockchain technology can be useful in this regard.
Another ethical issue related to digital health is the potential for bias and discrimination in AI and machine learning algorithms. These technologies rely on vast amounts of data to learn and improve, but if the data is biased or incomplete, the algorithms may produce inaccurate or discriminatory results. It is essential to ensure that these technologies are developed and implemented in a way that is fair and equitable for all patients, regardless of their race, gender, or socioeconomic status.
Finally, there is also the ethical issue of accessibility and equity. Digital health technologies have the potential to improve healthcare access and outcomes for many people, but they can also exacerbate existing health disparities if they are not accessible or affordable to all(MacFarlane, 2020). It is important to ensure that digital health technologies are developed and implemented in a way that is accessible and equitable for all patients, regardless of their income level or geographic location.
Overall, addressing ethical issues related to digital health is crucial to ensuring that these technologies can improve healthcare outcomes while also protecting patient privacy, promoting equity, and avoiding discrimination.
IV. Conclusion
In conclusion, digital and technological innovations have been and has further potential to transform healthcare delivery in India, by creating new opportunities for collaboration, learning, and innovation. From telemedicine and mobile health apps to remote patient monitoring and health information systems, these innovations have the potential to revolutionize healthcare delivery, particularly for marginalized populations who may face significant barriers to accessing traditional healthcare services.
It also made medical care more affordable by reducing the cost of medical services. For example, the use of telemedicine has reduced the cost of transportation and reduced the need for physical infrastructure. In addition, the use of digital technologies has led to better resource utilization, reduced administrative costs, and improved patient outcomes, leading to lower overall healthcare costs.
AI-based healthcare solutions, in particular, have shown promise in medical imaging analysis, personalized medicine, disease diagnosis and prediction, drug discovery, and patient monitoring. However, there are challenges to the widespread adoption of these solutions, including a lack of standardized data collection and management across different healthcare systems, as well as the need for regulatory frameworks to ensure that these solutions are safe, effective, and ethical.
But before the wide implementation of digital health platforms, it is important to address questions related to clinical effectiveness, reliability, and safety of these technologies. The implementation of digital health platforms should be based on evidence-based clinical research, which includes rigorous testing and validation of the proposed technologies. This ensures that the technologies are safe, effective, and reliable for use in healthcare.
Clinical effectiveness refers to the extent to which a digital health platform achieves its intended outcomes in a clinical setting. In addition, the reliability and safety of digital health innovations should be a top priority. This includes rigorous testing of the technologies to ensure that they are safe, secure, and reliable. This includes testing for potential cybersecurity vulnerabilities, as well as ensuring that the technologies comply with relevant privacy and security regulations. Furthermore, digital health innovations should be tested in accordance with ethical principles, including informed consent and protection of patient privacy.
Despite these challenges, ongoing investment and innovation in digital and technological innovations have the potential to significantly improve healthcare delivery and access in India and across the world, making it more accessible and equitable for all. In the end, it should be assured that these technologies should be used to bridge the social, economic and digital divide among the people and for benefit of all.
- Sayani, S., Muzammil, M., & Saleh, K. (2019). Addressing cost and time barriers in chronic disease management through telemedicine: an exploratory research in select low-and middle-income countries. Therapeutic Advances in Chronic Disease, 10.
- He, J. X., Baxter, S. L., Xu, J., Xu, J. M., Zhou, X. T., & Zhang, K. (2019). The practical implementation of artificial intelligence technologies in medicine. Nature Medicine, 25(1), 30-36.
- Wainstein, L. (n.d.). Telemedicine Trends to Watch in 2018.
- Mishra S, Kapoor L, Singh I. Telemedicine in India: Current scenario and the future. Telemed J E Health. 2009;15:568–75.
- Dasgupta A, Deb S. Telemedicine: A new horizon in public health in India. Indian J Community Med. 2008;33:3–8.
- United Nations Children’s Fund, ‘UNICEF Strategic Plan 2018–2021’, UNICEF, New York, January 2018, , accessed 10 March 2023.
- United Nations Children’s Fund Programme Division, ‘UNICEF’s Strategy for Health (2016–2030)’, UNICEF, 2015, , accessed 10 March 2023.
- Ashley RC. Telemedicine: legal, ethical, and liability considerations. J Am Diet Assoc. 2002 Feb;102(2):267-9.
- Hochgesang, M., Zamudio-Haas, S., Moran, L., Nhampossa, L., Packel, L., Leslie, H., Richard, J., & Shade, S.B. (2017). Scaling-up health information systems to improve HIV treatment: An assessment of initial patient monitoring systems in Mozambique. International Journal of Medical Informatics, 97, 322-330. doi: 10.1016/j.ijmedinf.2016.11.002.
- Mandal, S., Chadha, V.K., Laxminarayan, R., & Arinaminpathy, N. (2017). Counting the lives saved by DOTS in India: A model-based approach. BMC Medicine, 15(1), 47. doi: 10.1186/s12916-017-0809-5. PMID: 28253922; PMCID: PMC5335816.
- Hasselgren, A., Kralevska, K., Gligoroski, D., Pedersen, S. A., & Faxvaag, A. (2020). Blockchain in healthcare and health sciences-a scoping review. International Journal of Medical Informatics, 134.
- Brall, C., Schroder-Back, P., & Maeckelberghe, E. (2019). Ethical aspects of digital health from a justice point of view. European Journal of Public Health, 29(Supplement_3), 18–22.
- Hogaboam L, et al. Technology adoption potential of medical devices. Health Policy and Technology. 2018;7(3):273-280.
- van den Berg N, et al. Telemedicine and telecare for older patients—a systematic review. Maturitas. 2012;73(2):94-114.
- Singh H, Choudhury N, Singh N. Implementing National Digital Health Blueprint in India-The future opportunities and challenges. International Journal of Preventive Medicine. 2022;13(1):75. DOI: 10.4103/ijpvm.IJPVM_418_20.
- Palanisamy, V., and Thirunavukarasu, R. (2019). Implications of big data analytics in developing healthcare frameworks - a review. Journal of King Saud University-Computer and Information Sciences, 31(4), 415-425.
- Shafqat, S., Kishwer, S., Rasool, R. U., Qadir, J., Amjad, T., and Ahmad, H. F. (2020). Big data analytics enhanced healthcare systems: a review. The Journal of Supercomputing, 76(3), 1754-1799.
- Attia, Z. I., Kapa, S., Lopez-Jimenez, F., McKie, P. M., Ladewig, D. J., Satam, G., & Pellikka, P. A. (2019). Screening for cardiac contractile dysfunction using an artificial intelligence–enabled electrocardiogram. Nature medicine, 25(1), 70-74.
- Ashley, RC, Telemedicine: legal, ethical, and liability considerations. J Am Diet Assoc. 2002 Feb;102(2):267-9. doi: 10.1016/s0002-8223(02)90063-5. PMID: 11846125.
- A. MacFarlane, A., (2020) “General practice and the community: research on health service, quality improvements and training. Selected abstracts from the EGPRN Meeting in Vigo, Spain, 17-20 October 2019 Abstracts,” European Journal of General Practice, vol. 26, no. 1, pp. 42–50.
- International Telecommunications Union, ‘ICT Facts and Figures 2016’, ITU, , Available at: https://economictimes.indiatimes.com/industry/telecom/telecom-news/indian-to-have-820-million- smartphone-users-by-2022/articleshow/76876369.cms.
- Kraus, S, Schiavone F, Pluzhnikova A, Invernizzi AC. Digital transformation in healthcare: Analyzing the current state-of-research. Journal of Business Research. 2021;123:557-567.
- World Health Organization, Monitoring and Evaluating Digital Health Interventions: A practical guide to conducting research and assessment, WHO, Geneva, 2016, , accessed 11 March 2023.
